Overdose Prevention Centers Save Lives. Why Won’t Governor Hochul Authorize Them?
Across New York, overdose deaths are skyrocketing. But state officials are stalling on an evidence-based model that works.

Albany, NY—At the front of the rally, a middle-aged woman in a pink fur coat held a cardboard tombstone with a name: Jeff Dugan. Someone had also pasted two photographs on it: In one, Dugan is wearing a purple button-down shirt, smiling beatifically in front of a garden. In the other, he stands in a blonde-wood kitchen over a plate of food. The epitaph reads, “8-5-14. Forever 28. Our son, our brother, our chef.”
Alexis Pleus—Dugan’s mother and founder of Truth Pharm, a Binghamton-based harm reduction group—shouted, “If my son had a safe place to use, he might not have died alone in a bathroom!”
In April, 56 New York lawmakers—nine Republicans and four dozen Democrats—signed a letter sent to Governor Kathy Hochul, calling for her to declare a public health emergency over the overdose crisis. This, they argued, would allow her to waive copays for addiction treatment, increase Medicaid subsidies for treatment providers, and “enhance overdose prevention methods.”
Back in March, more than 100 harm-reduction advocates (including drug users themselves), lawmakers, healthcare workers, and family members of drug users rallied at the State Capitol to demand that Hochul expand overdose prevention centers, known as OPCs, in New York State. Activists held signs with numbers—over 3,800 lives could be saved—and organizers passed around cardboard tombstones with the portraits of loved ones.
Around 12:15 pm, after the rally had moved to the ground floor of the Capitol, we conducted a die-in in one of its busiest main hallways. One of the rally organizers led us in a meditation, summoning us to recall our lost loved ones and friends. I closed my eyes and sat with my knees up. I touched the marble floor and leaned my head back.
It was a few minutes of silence for us and passing lawmakers to reflect. I thought of my own sister, who, like Dugan, died alone. Analisa was an immigration attorney and only 30. She died of a fentanyl overdose on my childhood living-room couch in November 2016.
Overdose prevention centers are known by many names: safe injection sites, supervised consumption sites, safe injection facilities, and more. But the concept has been the same since the first official one opened in Bern, Switzerland, in 1986. There are at least 200 OPCs in over 14 countries. They’re places where drug users can bring, test, and use their own supply under the supervision of medical professionals, who can intervene with oxygen and opioid overdose reversal drugs like naloxone in the case of an overdose. Especially for the nearly four out of 10 OPC users in New York living on the streets, they offer showers, acupuncture, doctor’s appointments, housing referrals, STI and Hepatitis C testing, safety from street violence, and access to voluntary addiction treatment.
In their nearly 40 years of existence, no one has died in an OPC. In New York City—where the nonprofit OnPoint operates two of the nation’s only OPCs—OPC staff have reversed over 1,000 overdoses. International research supports that OPCs save lives, reduce public drug use in the neighborhoods around them, and increase access to life-saving treatment and care. One study conducted between 2017 to 2019, for instance, showed that in Toronto the communities near safe injection sites had the largest reductions in overdose mortality in the city.
The impetus for overdose prevention centers should not be a mother’s grief—or my own. For the last 10 years, the leading cause of accidental death in the United States has been overdose poisoning. The crisis is so severe that it’s caused a decline in life expectancy in the US. But there are steps that Hochul can take immediately to address the problem: She can declare a statewide medical emergency (or have her health commissioner do so), as several lawmakers and advocates have implored her to do, and she can finance new OPCs across the state using opioid settlement funds. By 2040, New York is set to receive $2.6 billion from opioid manufacturers and pharmaceutical companies.
Hochul most recently discussed her opposition to OPCs during a November 2023 press conference, where she said, “We are engaging in harm reduction strategies. There’s not only one. The ones that we’re doing are proven to be successful but also legal.” She revealed her apparent belief that OPCs violate state, local, and a particular federal law, known as the “crackhouse statute”—passed in 1986, the same year the first OPC was founded. This law prohibits any sites used for “selling, storing, or using” drugs.
A spokesperson for the governor wrote by e-mail, “All options need to be on the table to save lives, and we are working with experts and impacted communities to determine how best to reduce harm and keep New Yorkers safe,” reiterating that OPCs are not funded, operated, or overseen by New York State. The governor’s office declined to comment on the call for an emergency order on the overdose crisis.
Jasmine Budnella, director of drug policy for Voices of Community Activists and Leaders–New York, better known as VOCAL-NY, is steadfast in her belief that an executive order or legislation could legally expand OPCs. She points to a precedent from 1992, when then–health commissioner and head of the New York Department of Health Dr. Mark Chassin responded to the HIV crisis with an emergency order authorizing trained professionals at community organizations to possess syringes without a prescription. Syringe exchanges became legal in New York—despite federal funding for their remaining illegal—and HIV rates, especially among drug users, plummeted. “The governor’s argument is pretty flimsy,” she said. “She has the authority through the state’s Constitution to issue an executive order to authorize overdose prevention centers, and she can do that today.”
Another such pathway to authorization, Budnella said, is to pass the Safer Consumption Services Act, a bill that was introduced in 2017 and that would “establish a process for Overdose Prevention Centers to open and operate statewide.” The latest version of the bill calls for 10 OPCs statewide to be run in a five-year pilot program. It passed the Senate Health Committee May 7, in a 7-6 vote, and will move forward to the Senate Finance Committee next.
Authorizing OPCs through the Safer Consumption Services Act would allow the governor to build a “regulatory framework” around them, and “allow for city and state dollars” as well as opioid settlement funds to support them, Budnella said.
One state has already green-lighted OPCs. In July 2021, Rhode Island’s state legislature passed a law allowing for the creation of a research-backed OPC, as part of a pilot program between Brown University’s School of Public Health and NYU’s Langone Health Center. In February 2024, after many meetings between state and local officials, community members, nonprofits, and lawmakers, the Providence City Council unanimously supported the bill, and the nonprofit Project Weber/RENEW is set to operate the space. The nation’s first state-sanctioned OPC is slated to open in Providence in fall 2024, and will use at least $2 million from opioid settlement dollars.
The only two OPCs in New York City—and the only two nationwide—opened thanks to a coordinated agreement facilitated by then-Mayor Bill DeBlasio in November 2021. DeBlasio and NYC’s Health Department decided that the best course of action to reduce opioid deaths would be to open an OPC within a successful syringe service program that had a long-standing relationship with its surrounding community. The city chose OnPoint as the pilot site, with its locations in East Harlem and Washington Heights. The city and agencies then organized a series of discussions with local, state, and federal representatives to convince them of the urgency and effectiveness of OPCs. The Department of Health even sent senior NYPD officials and some of the city’s district attorneys to Europe and Canada, so they could visit OPCs and see how the model worked and would be implemented in New York City.
Finally, after consolidating support among City Council members, law enforcement, and the community, DeBlasio wrote a letter to OnPoint, pledging that law enforcement and the district attorneys from Manhattan, Brooklyn, Queens, and the Bronx would support their operations, a commitment that allows OnPoint’s sites to remain open to this day.
Similar to the case of Rhode Island, what made New York City’s OPCs possible was research that reinforced that OPCs were cost-effective and life-saving: a feasibility study that showed that overdose deaths could be mitigated by expanding OPCs into existing syringe service programs across the city. In 2018, bowing to advocates’ pressure, DeBlasio released the results of the study, which indicated that four OPCs would save more than 130 lives and up to $7 million in healthcare costs each year.
Aside from discounting the local and state victories of OPCs in New York City and Rhode Island, Hochul’s inaction in supporting OPCs also runs counter to the recommendations of the state’s Opioid Settlement Fund Advisory Board. For the past two years, the OSF Advisory Board has advocated that some of the settlement funds be used to support OPCs through a research pilot program in both urban and rural areas.
One of the hurdles to opening more OPCs are the assumptions that many people have about them. Toni Smith, the New York State policy director at Drug Policy Alliance, told me that OnPoint’s OPC staff are “pretty gracious” when politicians or community leaders visit and remark on how shocked they are at how normal the places seem.
Visitors’ surprise raises a question underlying so much of this crisis: How do you expect a drug user to look? “The person who is forced to hide in a public setting—behind a building, or in an alley or a staircase—who needs to rush, who needs to fear being punished, criminalized, or captured on camera,” Smith said, “is going to look very different in a setting where they are allow to sit, feel comfortable, and be themselves.”
The War on Drugs—specifically New York’s Rockefeller Laws passed in 1973—effectively criminalized drug users. Anyone caught possessing even a small amount of marijuana, cocaine, or heroin would receive a mandatory prison sentence of 15 years to life. Teenagers caught selling drugs would be treated as adults in the legal system.
The laws hollowed out families and communities. According to the Physicians for Human Rights and the Fortune Society, which conducted interviews with 50 men and women incarcerated for nonviolent drug offenses in New York, “Families lose sons, brothers, husbands and fathers; communities lose potential leadership and economic power, schools lose parental involvement.”
These laws led to prolonged economic disinvestment in already impoverished neighborhoods, exacerbated addiction and crime rates, and worsened the disproportionate incarceration rates among Black and Latino New Yorkers. Felony drug arrests rose from nearly 15,000 in 1973 to more than 62,000 in 1989. By 1992, 5 percent of individuals incarcerated through drug-related felonies were white, 50 percent were Black, and 44 percent were Latino, even though the rates of illicit drug use in New York State have historically been highest in white communities.
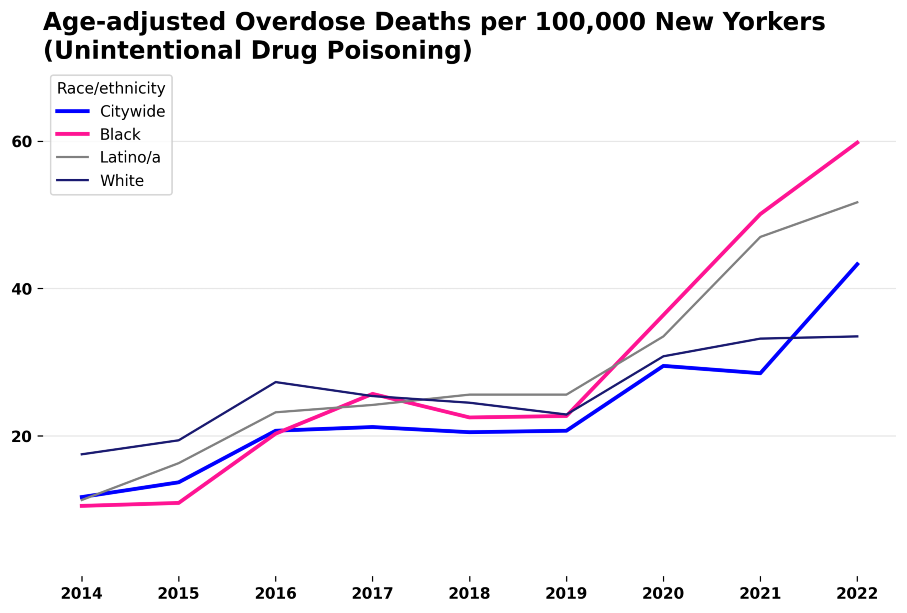
The criminalization of the War on Drugs also coincided with increased drug use, as the crack epidemic decimated urban communities of color. Black and Latino New Yorkers suffered higher rates of IV drug use, and their overdose death rate remains disproportionately high. For every 100,000 Black New Yorkers, about 62 die of overdoses every year, nearly double the rate of their white counterparts. Latino New Yorkers died at the second-highest rate, at 53.1 per 100,000.
Popular
“swipe left below to view more authors”Swipe →Drug criminalization also contributes to overdose deaths through the “iron law of prohibition.” According to this principle, a criminalized substance’s quality becomes more lethal as a black market emerges. Steven Gray, a drug policy organizer at VOCAL-NY, told me this is worsening the current overdose crisis, in which fentanyl and xylazine contaminate the drug supply and cause fatal overdoses. Gray said fentanyl and xylazine-laced drugs are the modern equivalent of lethal “moonshine during Prohibition,” a time when bootleg alcohol killed approximately 1,000 Americans a year.
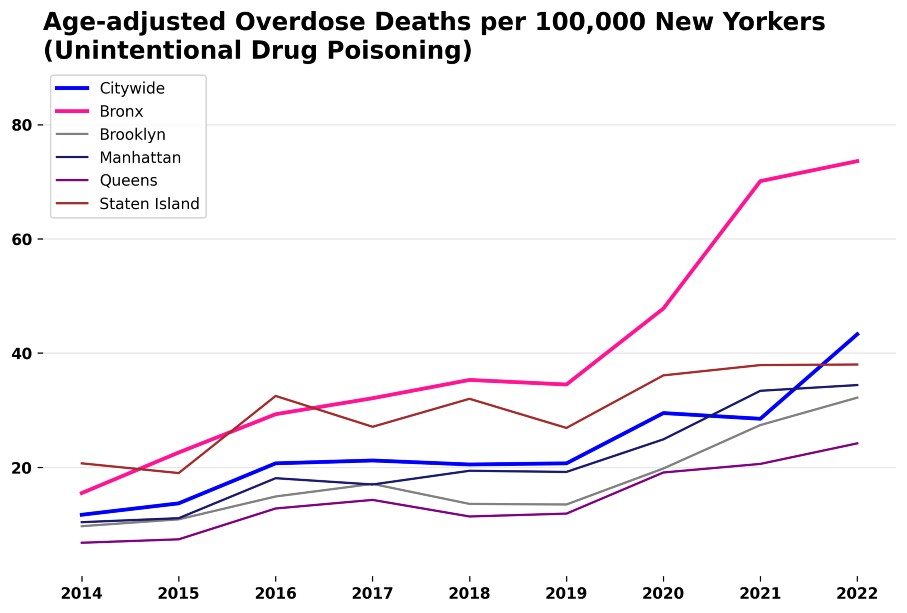
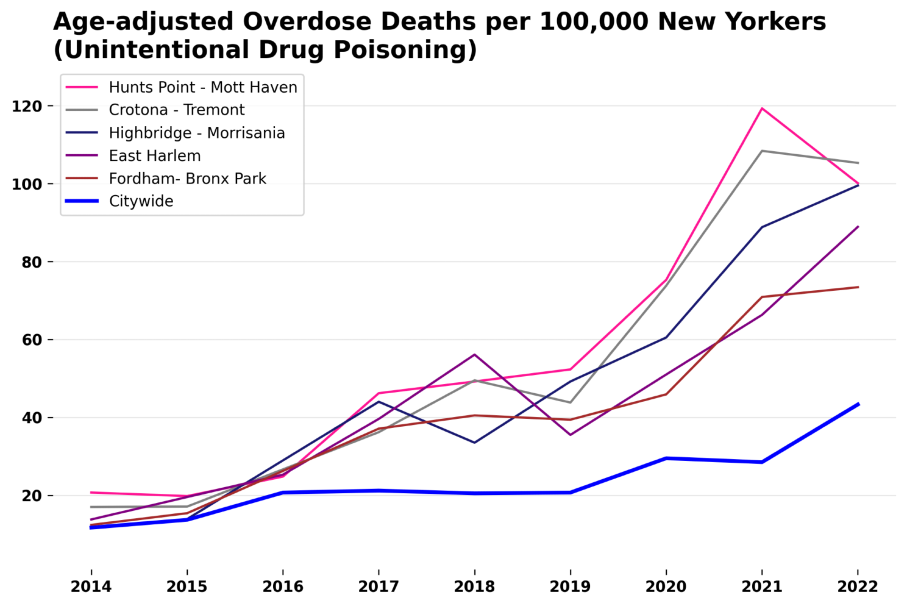
This has made the crisis especially urgent in the Bronx, where overdoes rates far exceed the national average. In the Crotona-Tremont area of the Bronx, about one in 1,000 residents dies of an overdose every year.
The need for accessible OPCs in the Bronx in particular is acutely felt by harm reduction advocates. “Drug users who are destitute don’t have $6 for the round trip to go to the OPC,” said Camila Gelpi-Acosta, a sociologist and professor, referring to OnPoint’s locations in Manhattan. “If you’re injecting 15 times a day, are you going to go 15 times from the Bronx? It doesn’t make any sense.”
Gustavo Rivera has been a state senator representing district 33 in the Bronx since November 2010, and has been a member of the Joint Senate Task Force on Opioids, Addiction, and Overdose Prevention since it formed in July 2019. He is also one of the original cosponsors of the Safer Consumption Services Act. He told me that when he was recently asked if he’d want an overdose prevention center in his own backyard, he didn’t miss a beat: “I answered, ‘Absolutely,’ I would want one here tomorrow.”
Rivera said he doesn’t balk at community members concerned about bringing their kids to school and passing drug users who are shooting up. He said he hears them out but offers harm reduction policy ideas they don’t always want to hear.
“You can’t tell me that you don’t want to see ‘those people’ in your way when you’re trying to get to the train station and that you are opposed to opening up a facility in which they can—under medical supervision and in a safe environment—use privately,” he told me. “Some people would argue, ‘Just put them away. Just throw these people away. As long as I don’t see them, they’re not a problem.’ This is not some foreign agent that’s coming to invade us. These are people from our backyard, who have a medical problem. So let’s deal with it as a public health issue and respond to it with a public health policy.”

In September 2023, I visited OnPoint’s OPC in East Harlem, located in a nondescript brick building. I met Susan Spratt, the associate director of clinical services, who told me that OnPoint’s clinic is open to anyone regardless of insurance. Hepatitis C testing and treatment as well as buprenorphine and suboxone administration are two of the biggest services.
“A lot of our folks are people who have been obviously stigmatized for their drug use, and they’re people whose medical needs have not been met ever or for a very, very long time,” Spratt said. “We’re not a primary care clinic, but we have a lot of people coming in with issues that would be characterized as primary care needs.”
One of driving principles at OnPoint is the importance of educating its patients. The organization believes drug users should have the self-determination and information they need to be safe. “You’re trying to give people as much knowledge as they can to mitigate whatever harms might occur with what they’re doing,” she said.
I then traveled up a few flights to speak with Sam Rivera, the executive director of OnPoint, about the precarity of OPCs. Only a month prior, a federal prosecutor, Damian Williams, had threatened to shut down OnPoint’s OPCs, claiming they violate local, state, and federal law. But Rivera (no relation to Gustavo Rivera) remained optimistic. He said he received calls and letters from across law enforcement and the federal government in support of what the OPCs have done and been able to achieve. He said it ultimately reinforced the success of OnPoint, and brought him even more faith that the model is saving lives and shifting perceptions.
Rivera said he believes the family-like community he’s helped foster speaks for itself and that his door is always open. But neither Hochul nor Williams has visited an OPC. “Right now, she’s failing us,” Rivera said of the governor. “It’s sad that we’ve been here almost two years. Where have you been?” But then, Rivera quickly returned to his signature cheerfulness. After all, he’s seen people embrace OPCs when they understand what they can accomplish, and he refused to count out Hochul. “I believe she’s going to change. I really do.”
More from The Nation

What Luigi Mangione and Daniel Penny Are Telling Us About America What Luigi Mangione and Daniel Penny Are Telling Us About America
When social structures corrode, as they are doing now, they trigger desperate deeds like Mangione’s, and rightist vigilantes like Penny.
Banning Trans Health Care Puts Young People at Risk of Harm Banning Trans Health Care Puts Young People at Risk of Harm
The Supreme Court will increase risks by upholding state bans on gender-affirming care, contrary to what conservative lawmakers argue.
It’s Still Not Too Late for Biden to Deliver Debt Relief It’s Still Not Too Late for Biden to Deliver Debt Relief
Four years after hearing the president promise bold action on student debt, most borrowers are still no better off, and many—especially defrauded debtors—are measurably worse off....

It’s Been a Tough Year. Let’s Help Each Other Out. It’s Been a Tough Year. Let’s Help Each Other Out.
There may be a dark shadow hanging over this year’s holiday season, but there are still ways to give to those in need.

Prison Journalism Is Having a Renaissance. Rahsaan Thomas Is One of Its Champions. Prison Journalism Is Having a Renaissance. Rahsaan Thomas Is One of Its Champions.
Thomas and his colleagues at Empowerment Avenue are subverting the established narrative that prisoners are only subjects or sources, never authors of their own experience.

Luigi Mangione Is America Whether We Like It or Not Luigi Mangione Is America Whether We Like It or Not
While very few Americans would sincerely advocate killing insurance executives, tens of millions have likely joked that they want to. There’s a clear reason why.


