In the US, Mental Health Treatment Can Be a Death Sentence
Deploying the language of “helping” those in need, policymakers are reaching not for a Band-Aid but a club.
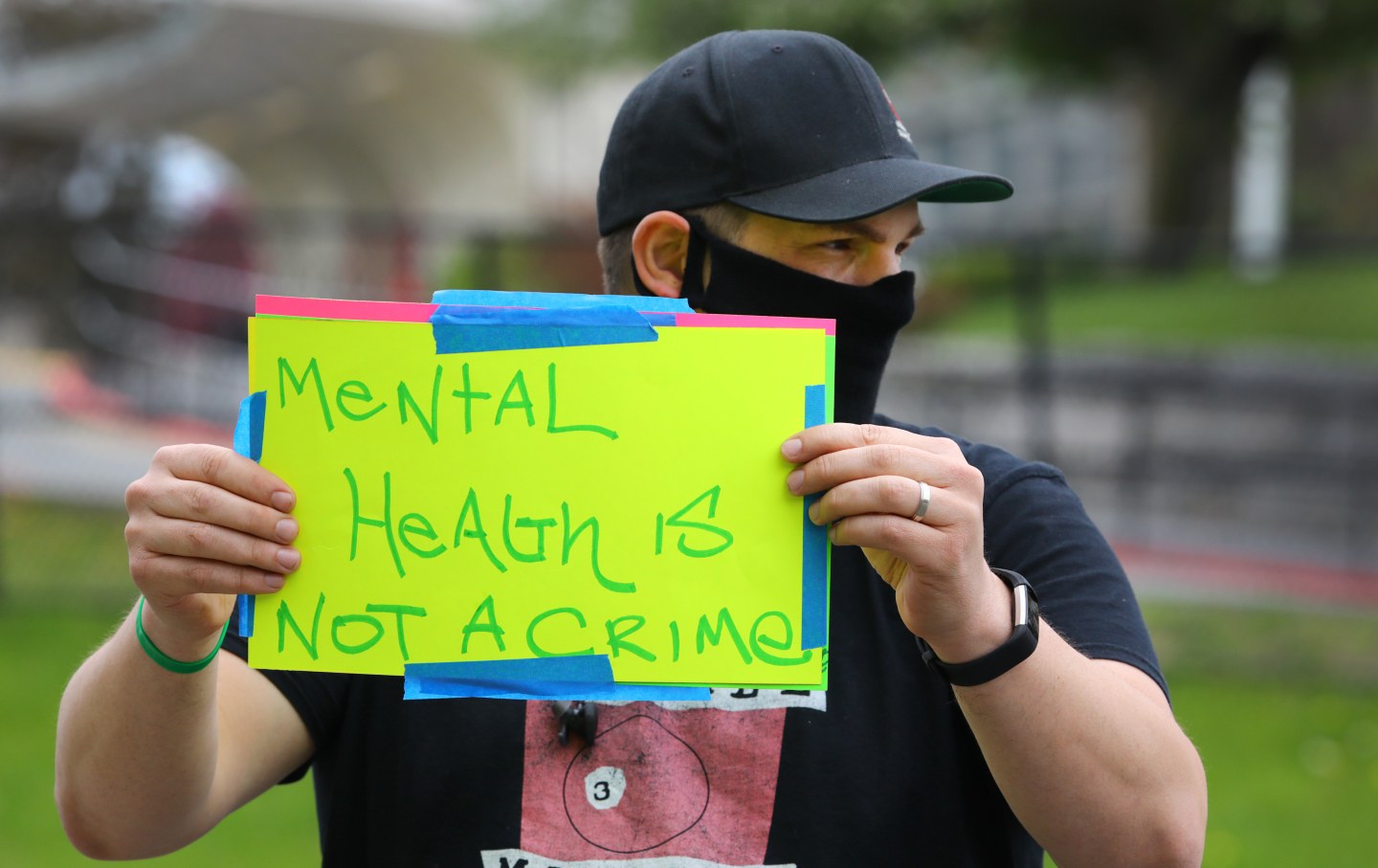
Jason Wright holds a sign reading “mental health is not a crime” in Boston on May 17, 2020.
(Pat Greenhouse / The Boston Globe via Getty Images)This article originally appeared at TomDispatch.com. To stay on top of important articles like these, sign up to receive the latest updates from TomDispatch.com.
Amid ongoing emergencies, including a would-be autocrat on his way to possibly regaining the American presidency and Israel’s war on Gaza (not to mention the flare-ups of global climate change), the United States has slipped quietly toward an assault on civil liberties as an answer to plummeting mental health. From coast to coast, state lawmakers of both parties are reaching for coercive treatment and involuntary commitment to address spiraling substance use and overdose crises—an approach that will only escalate despair and multiply otherwise preventable deaths while helping to choke the life out of America.
In December, we wrote about how loneliness has become a public-health crisis, according to the Surgeon General, and the ways in which it drives widespread substance use. We reach for substances to ease feelings of isolation and anguish—and when the two of us say “we,” we mean not just some hypothetical collective but the authors of this article. One of us, Sean, is a doctor living in long-term recovery from a substance-use disorder and the other, Mattea, is a writer who uses drugs.
And we’re anything but unique. Disconnection and loneliness aren’t just the maladies of a relatively few Americans, but the condition of the majority of us. Vast numbers of people are reaching for some tonic or other to manage difficult feelings, whether it’s weed, wine, work, television, or any mood- or mind-altering substance. These days, there’s scarcely a family in this country that’s been unscathed by problematic drug use.
Not surprisingly, under the circumstances, many elected officials feel increasing pressure to do something about this crisis—even as people who use drugs are widely considered to be social outcasts. In 2021, a survey of thousands of US-based web users found that seven in 10 Americans believed that most people view individuals who use drugs as non-community members. It matters little that the impulse to use such substances is driven by an urge to ease emotional pain or that the extremes of substance use are seen as a disease. As a society, we generally consider people who use drugs as rejects and look down on them. Curiously enough, however, such social stigma is not static. It waxes and wanes with the political currents of the moment.
“Stigma has risen its ugly head in almost every generation’s attempts to manage better these kinds of issues,” says Nancy Campbell, a historian at Rensselaer Polytechnic Institute and the author of OD: Naloxone and the Politics of Overdose. Campbell reports that she finds herself a target of what she calls “secondary stigma” in which others question why she even bothers to spend her time researching drug use.
Perhaps one reason to study such issues is to ensure that someone is paying attention when lawmakers of virtually every political stripe seek to answer a mental health crisis by forcing people into institutionalized treatment. Notably, such “treatment” can increase the odds of accidental death. Allow us to explain.
“Treatment” Can Be a Death Sentence
Across the country, the involuntary detainment and institutional commitment of people with mental illness—including those with a substance use disorder—is on the rise. Deploying the language of “helping” those in need, policymakers are reaching not for a band-aid but a club, with scant or even contradictory evidence that such an approach will benefit those who are in pain.
“The process can involve being strip-searched, restrained, secluded, having drugs forced on you, losing your credibility,” said UCLA professor of social welfare David Cohen in a 2020 statement about his research on involuntary commitment. He co-authored a study that found its use rose nationwide in the decade before the pandemic hit, even as there was a striking lack of transparency regarding when or how such coercion was used.
Today, many states are expanding laws that authorize mandatory treatment for people experiencing mental-health crises, including addiction. According to the Action Lab at the Center for Health Policy and Law, 38 states currently authorize involuntary commitment for substance use. None of them require evidence-based treatment in all involuntary commitment settings and 16 of them allow facilities to engage in treatments of their choice without the individual’s consent. Nearly every state that ranked among the highest in overdose rates nationally has an involuntary commitment law in place.
In September, the California legislature passed a bill that grants police, mental healthcare providers, and crisis teams the power to detain people with “severe” substance use disorder. The Los Angeles County Board of Supervisors subsequently voted to postpone implementation of the law, with Board Chair Lindsey Hogarth noting the risk of civil rights violations as a reason for the delay. In October, Pennsylvania state legislators introduced a bill that would permit the involuntary commitment of people who have been revived following an overdose. While many mental health advocates acknowledge the good intentions of legislators, the potential for harm is incalculable.
New research shows that people who attended abstinence-based treatment programs were at least as likely, if not more likely, to die of a fatal overdose than people who had no treatment at all. By contrast, those who had access to medications like methadone or buprenorphine for opioid-use disorder were less likely to die. Those medications, however, are not considered “abstinence” and so are not uniformly provided in treatment settings. Though there is extensive evidence of the effectiveness of medications for opioid use disorder, abstinence still remains widely regarded as the morally upright and best path, even if it makes you more likely to die. The reason for the elevated risk of mortality following abstinence-based treatment is no mystery: abstinence reduces the body’s tolerance. If a person who has been abstinent resumes use, the ingestion of a typical dose is more likely to overwhelm his or her bodily system and so lead to death.
Disturbingly, both The Atlantic and The Wall Street Journal recently ran columns favoring mandatory treatment, with the Journal citing as evidence a 1960s study in which individuals fared well after 18 months of mandated residential treatment that included education and job training—a standard of care that’s virtually nonexistent today. The Atlantic referenced a study of 141 men mandated for treatment in the late 1990s whose outcomes were comparable to individuals who entered treatment voluntarily; the study’s own authors had, however, cautioned against generalizing the findings to other populations due to its limited scope—and since then, the potent opioid fentanyl has entered the drug supply and raised the risk of a fatal overdose following a period of abstinence.
Popular
“swipe left below to view more authors”Swipe →Meanwhile, as policymakers turn to coerced treatment, consider this an irony of the first order: there are far too few treatment options for people who actually want help. “There is no place in this country where there is enough voluntary treatment. So why would you create involuntary commitment, involuntary treatment?” asks Campbell. The reason, she suggests, is the inclination of lawmakers not just to do something about an ongoing deadly crisis, but in no way to appear “soft on drugs.”
Just to put the strange world of drug treatment in context, imagine elected officials wanting to seem tough on constituents who have cancer or heart disease. The idea, of course, is ludicrous. But seven in 10 Americans think society at large views addiction as “at least somewhat shameful” and people who use drugs as significantly responsible (that is, to blame) for their substance use. No surprise, then, that politicians would find it expedient to punish people who use drugs, even if such punishment only layers on still more shame, with research indicating that shame, in turn, exacerbates the pain and social isolation that drives people to use drugs in the first place. As Dr. Lewis Nelson, who directs programs in emergency medicine and toxicology at Rutgers New Jersey Medical School, pointed out to USA Today, the science of addiction and recovery is frequently overlooked because it’s inconsistent with ingrained social ideas about substance use.
“I Still Don’t Need Saving”
Punishing people for substance use worsens the pain and isolation that make drugs so appealing. So rather than punishment—and in our world today this will undoubtedly sound crazy—what if we treated people who use drugs as full and complete human beings like everyone else? Like, say, people with high blood pressure? What if we acknowledged that those who use drugs need the very same things that all people need, including love, support, and human connection, as well as stable employment and an affordable place to live?
Research on this, it turns out, suggests that human connection is particularly good medicine for the emotional pain that so often underlies substance use and addiction. Stronger social bonds—namely, having people to confide in and rely on—are associated with a positive recovery from a substance use disorder, while the absence of such social ties elevates the risk of further problematic drug use. Put another way, perhaps you won’t be surprised to learn that a powerful means of healing widespread mental distress is to connect with one another.
When people in distress have friends, attendant family, and healthcare providers who are genuinely there for them no matter what, their own self-perception improves. In other words, we help one another simply by being nonjudgmentally available.
Jordan Scott is a peer advocate for Recovery Link, which offers free digital peer support to people in Texas and Pennsylvania. She identifies as a person who uses drugs. “I felt like the message got reinforced that there was something wrong with me, that there was something broken with me,” she told us. “Anything that isn’t abstinence, or anything that doesn’t include total abstinence as a goal, is constantly positioned as less than.”
New research published in the journal Addiction draws a contrast between treatment focused exclusively on abstinence and a broader array of wellness strategies, including reducing drug use rather than eliminating it entirely. The study found that reduced use had clinical benefits and that health can distinctly improve even without total abstinence. Director of the National Institute on Drug Abuse Nora Volkow, for instance, supports a nuanced approach that includes many possible paths of recovery along with a shift away from the criminalization of drug-taking to a focus on overall health and wellbeing. And the Substance Abuse and Mental Health Services Administration, a branch of the US Department of Health and Human Services, has identified four dimensions critical to recovery: health, home, purpose, and community.
Most important of all, a person doesn’t necessarily need to be abstinent in order to make gains in all four areas. This makes good sense when you remember that addiction or other problematic substance use is a symptom of underlying pain. Rather than exclusively treating the symptom—the drug use—addressing the underlying loneliness, trauma, or other distress can be a very effective approach. “Family can be a valid pathway to wellness,” Scott pointed out, while adding that her own path went from 12-step meetings like Alcoholics Anonymous to active civic engagement.
For someone else, quality time with his or her kids or even exercising and eating well might be a linchpin for staying mentally healthy. In other words, healing from the pain that underlies substance use disorder can look a lot like healing from any other health challenge.
Yet policymakers continue to call for intensifying the use of coercive treatment. “I think we’re going to see more [involuntary commitment] before we see less of it,” said Campbell, who studies historical patterns in the social response to drug use. There’s nothing new, she noted, in the move to “help” people by institutionalizing them—even if such a move constitutes an erosion of basic civil rights.
“I think most of the time people are genuine in wanting to help,” said Scott, who has been a target of such “help.” The problem, she explained, is the idea that there is a group of people considered “normal” and therefore superior, who think they’re in a position to save other members of society.
“I didn’t need saving. I am a drug user now. I still don’t need saving,” Scott told us. These days she’s focused on being a part of her community through volunteerism while drawing on a support network of people who respect her path.
As for the two of us writing this article, Sean is spending time with his children, staying connected with friends, practicing meditation and yoga, and has for years facilitated a group of physicians in recovery. Mattea has started a new habit of going to the gym with her uncle to ease her loneliness, while also confiding in close friends for support. And all of that truly does make a difference.
More from The Nation

What Luigi Mangione and Daniel Penny Are Telling Us About America What Luigi Mangione and Daniel Penny Are Telling Us About America
When social structures corrode, as they are doing now, they trigger desperate deeds like Mangione’s, and rightist vigilantes like Penny.
Banning Trans Health Care Puts Young People at Risk of Harm Banning Trans Health Care Puts Young People at Risk of Harm
Contrary to what conservative lawmakers argue, the Supreme Court will increase risks by upholding state bans on gender-affirming care.
It’s Still Not Too Late for Biden to Deliver Debt Relief It’s Still Not Too Late for Biden to Deliver Debt Relief
Four years after hearing the president promise bold action on student debt, most borrowers are still no better off, and many—especially defrauded debtors—are measurably worse off....

It’s Been a Tough Year. Let’s Help Each Other Out. It’s Been a Tough Year. Let’s Help Each Other Out.
There may be a dark shadow hanging over this year’s holiday season, but there are still ways to give to those in need.

Prison Journalism Is Having a Renaissance. Rahsaan Thomas Is One of Its Champions. Prison Journalism Is Having a Renaissance. Rahsaan Thomas Is One of Its Champions.
Thomas and his colleagues at Empowerment Avenue are subverting the established narrative that prisoners are only subjects or sources, never authors of their own experience.

Luigi Mangione Is America Whether We Like It or Not Luigi Mangione Is America Whether We Like It or Not
While very few Americans would sincerely advocate killing insurance executives, tens of millions have likely joked that they want to. There’s a clear reason why.


