Welcome to the Age of Psychedelic Inequality
Psychedelic-assisted therapies have been hailed as the wave of the future. They’re also becoming big business. What if most people can’t afford them?
It was an early summer morning, and Katy had been up for most of the night. During those hours, she had experienced what she would later describe as some of the most fantastical things she had ever seen in her 52 years. She had taken a psilocybin “journey” in the desperate hope of severing her addiction to alcohol, and she was now sitting on the floor in a house in a Colorado suburb, surrounded by six facilitators and 12 strangers. She was thinking about all that had led her to this point.
Katy had recently left jail and was on probation after being arrested and charged eight months earlier for alcohol intoxication. She had been sitting in her parked car, alternating whiskey with the hard seltzer White Claw, when a bank worker alerted the police to her presence. Later, watching the police cam footage from her arrest, Katy would see herself pleading, crying, and ultimately getting belligerent with the officers.
Before her brush with the law, Katy’s life had been marked by constant drinking, which now filled her with regret. She felt she hadn’t taken the best care of her kids—an opinion that her 20-year-old daughter, who had stopped talking to her after her arrest, appeared to share. Katy was willing to do almost anything to change.
This eagerness to confront her addiction was part of what had propelled her to participate in that night’s psilocybin ceremony. It is also what made her willing to pay the $400 fee for this group trip (the standard fee was $600, but Katy got a $200 break), which she put on her credit card, along with the fee for a previous foray into ketamine therapy, where it joined the rest of the debt that weighs her down (Katy’s home-cleaning business earns her just $30,000 to $40,000 a year). But even so, she insisted it was worth it. From twilight to the next morning, she had experienced something “incredible,” and somehow it had stanched her desire for alcohol and eased the profound dread that led her to drink in the first place. She believed in the experience so fervently, she later paid another $450 to attend an ayahuasca ceremony. Four months later, she felt like she had a better understanding of her addiction, and that new understanding gave her hope that she might finally recover from it. “The beginning of healing is awareness,” she says now.

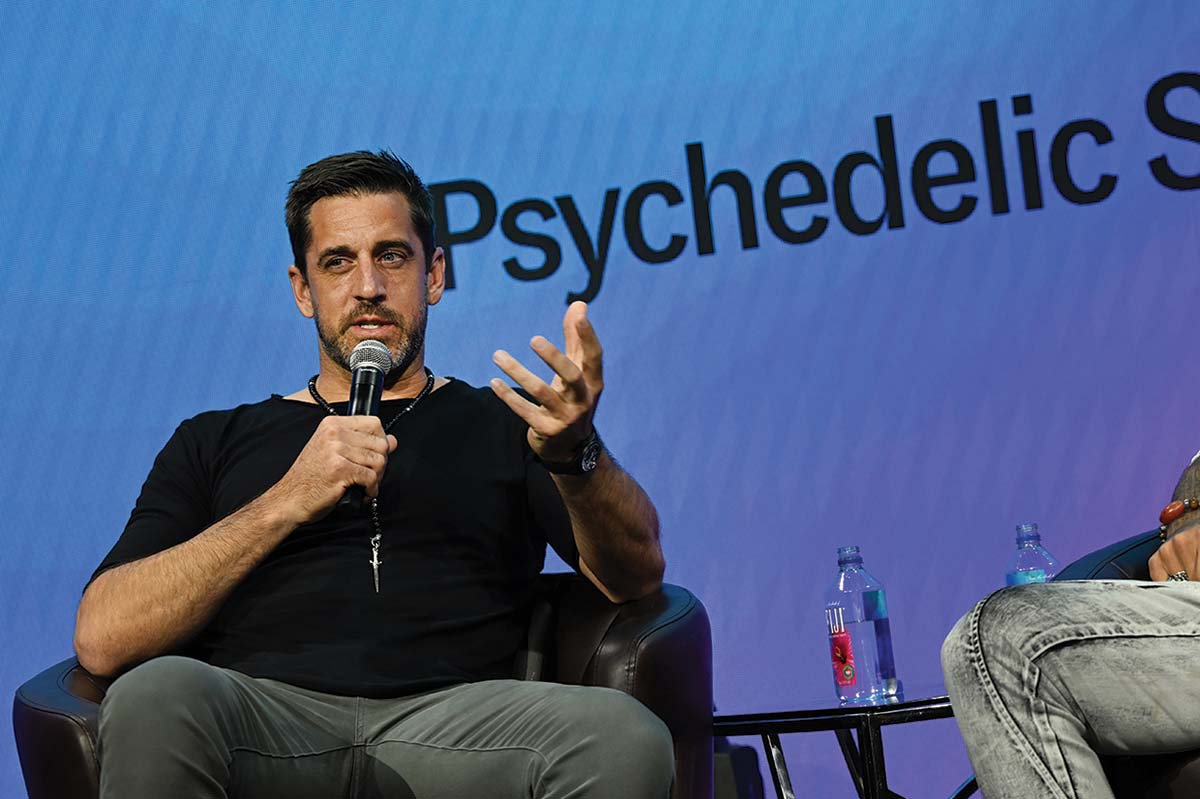
Katy is one of a growing number of Americans who have turned to psychedelic-assisted therapy and found it to be something close to a panacea, the first thing that has ever led to a lasting sense of transformation. The therapies include a range of psychoactive substances, from psilocybin to MDMA to LSD to ketamine. (Though ketamine is a dissociative anesthetic, it can induce altered states and is generally classed among the new psychedelic-assisted therapies.) Most of these drugs, which have long been criminalized, have generally been perceived as little more than hippie diversions or club-kid scourges. But over the past decade, there has been a shift in thinking toward the recognition of their potential use in powerful therapeutic interventions. In the past five years, this perspective has migrated closer to the mainstream, as everyone from writers like Michael Pollan (whose How to Change Your Mind helped open the floodgates) to mental health advocates to business bros has begun singing the gospel of psychoactive therapy.
This rosy view is supported by a growing body of evidence. Tantalizing research suggests that hallucinogens and similar drugs may be able to ease or even cure post-traumatic stress disorder, addiction, depression, and many other psychiatric disorders, sometimes in just a few sessions. In the case of MDMA, for instance, a 2021 multisite study that explored its use to treat PTSD found that the drug, when accompanied by psychotherapy sessions, was “highly efficacious”: It led to the remission of PTSD symptoms at twice the rate of the placebo, as well as “loss of diagnosis” at twice the rate—results echoed by those of a similar study published in 2023. Also in 2021, The New England Journal of Medicine published robust results from a study on the use of psilocybin, alongside psychotherapy, to treat long-standing depression. While these and other studies have tended to be small, and almost all emphasize the need for simultaneous therapy, the findings have been promising enough that the Food and Drug Administration has granted “breakthrough therapy” designation to MDMA and psilocybin for PTSD and serious depression, respectively. (The “breakthrough therapy” designation is designed to speed the development and review of promising drugs.)
Even as the promise of psychedelic treatments has grown, however, so too has the price, leaving many people who could benefit from these therapies unable to afford to take part in the psychedelic renaissance. As the nonprofit Psychedelic Access Fund has noted, one session of psilocybin therapy tends to run between $1,500 and $3,500, while attendance in an MDMA program (typically three six- or eight-hour sessions with a therapist while on the drug and then several additional therapy sessions without it) costs $11,000 to $15,000. Ketamine, one of the only treatments that is legal, can run between $400 and $800 per session, even though the drug itself can cost as little as $10. Even group therapy settings, which tend to be the most affordable, are out of reach for most; one psychedelic therapy advocate, Claudia Cuentas, the cultural director of the Alma Institute in Portland, Oregon, estimated that the best rate for a single session of group psilocybin therapy can still run as high as $800 (and often more).
Meanwhile, wealthy people have no trouble getting access to psychedelics. Experience-chasing one-percenters enjoy $1,300-a-head shamanic ritual experiences or house parties spiced up with postprandial dabbling. Or they can just hand over the hundreds for a single ketamine or psilocybin session.
For these well-heeled wellness seekers, the fact that most of these therapies aren’t covered by health insurance—a legacy, in part, of the drugs’ long-criminalized status—is no deterrent. They’re fine paying thousands of dollars out-of-pocket. But for the majority of potential patients, the lack of insurance coverage is a serious challenge: It’s one of the prime reasons they can’t pay the sky-high prices, and it’s the difference for all too many between getting treatment and forgoing it, or between getting treatment and going into debt for it. This is true even for treatments like psilocybin, which is now legal to use in Colorado and Oregon, and ketamine, which is both legal and approved by the FDA, but only for use as an anesthetic, meaning that its use to treat trauma or depression is considered “off-label” by insurance companies. In both cases, lower- and middle-income Americans are once again shut out.
But the problem goes beyond insurance. As psychedelics have emerged from the underground, they’ve been swept up in an investor bonanza. Eager to turn therapeutic promise into corporate profits, billionaires like Peter Thiel have gotten in on the action, infusing money into biotech start-ups racing to patent new psychedelic compounds, while pharmaceutical companies scramble to concoct their own psychedelic treatments. Some analysts predict that the psychedelics industry could be worth as much as $8 billion within four years. The investing frenzy isn’t limited to the drugs themselves, either. You can see the speculative hype in the ketamine clinics that have begun popping up around the country, as well as in the range of artisanal products—think psilocybin-infused honey—that are suddenly being marketed to moneyed consumers. You can see it in the rise of lifestyle entrepreneurs whose far-flung psychedelic retreats give new meaning to “high”-end luxury travel. For $7,000, customers can combine the thrill of a psychedelic trip with the pampered pleasures of a Caribbean one at any of the new psychedelic retreats popping up in vacation spots like Jamaica and Costa Rica.
Parallel to this one-percenter-driven capitalist exuberance, however, is ordinary citizens’ deprivation. While tech bros enjoy microdosing work retreats and celebrities learn a “deeper self-love” through ayahuasca journeys, those working- and middle-class Americans who crave treatment are left grasping like Tantalus at fruit that is always just out of reach. Many of these Americans are the very ones for whom access to quality mental health treatment is historically most scarce—and most vital.
In a 2021 article in the International Journal of Drug Policy, Kerri Rea and Bruce Wallace came perhaps as close as any academics can to sounding an alarm about this dawning access gap: “The novel and inchoate acceptance of psychedelic-assisted therapies into mainstream medical and therapeutic realms raises questions of equity. Concerns have been raised that individuals and communities facing structural inequities are perhaps least able to access these treatments including Black, Indigenous and people of colour (BIPOC) as well as people who use drugs.” And they concluded: “Psychedelic-assisted therapies may exemplify the inverse law of care whereby services are most inaccessible to communities with the most need.”
Psychedelic medicine is fast becoming big business. In the coming years, more (if not all) of the drugs used in psychedelic therapies may well be legalized. That’s good news for those lucky enough to be able to afford the treatments. But where does that leave the rest of us?
Over the past few years, I’ve gone on my own “journey,” to use the psychedelic parlance, to better understand who is being left out of the promise of the psychological healing that such therapy can offer. Some of this research has involved eating attractively packaged psychedelic chocolates at a cocktail party or having conversations at other bougie gatherings with therapists who eagerly mention that they’ve added ketamine lozenges to their practice. But some efforts have been more serious. Two years ago, I called around looking for a therapist who would be open to offering psychedelic treatment for a longtime sleep disorder I’ve struggled with—one that I believe is linked to trauma. Years of psychotherapy and even psychoactive medication hadn’t addressed these tenacious sleep issues, including sleep talking and, even more disconcertingly, sleepwalking (I might find myself in a different room from the one I went to sleep in, for example, and not remember how I got there). Nor had I found relief in a sleep study, which failed to culminate in my dreams involving, say, being chased by half-men, half-deer; instead, I could barely sleep with the octopus of wires and sensors attached to my head.
Psychedelics, in contrast, seemed to hold real promise. I’d heard stories of the remarkable recovery of people with PTSD using psychedelic therapies, narrated as if these drugs were the equivalent of the laying-on of hands. I had heard that MDMA, sometimes called ecstasy, could help me, especially if it was delivered in an appropriate setting with skilled facilitators. The problem was the prices I was quoted, averaging $800 for just one session.
Then I heard that the largest clinical trial of MDMA to date was recruiting people with PTSD for the third and final phase of its study. The trial was being conducted by the Multidisciplinary Association for Psychedelic Studies, or MAPS, a research, education, and advocacy nonprofit that has been at the forefront of the push for psychedelic therapy since 1986. I had read promising reports about other MDMA studies, and I was eager to find out for myself.
So when someone sent me an e-mail about applying for the MAPS study, I embarked on the lengthy audition for admission. I went to a glamorous intake site—mid-century modern with acid-trip-inspired throw pillows. I also sat for a number of sessions with a study psychiatrist, filled out a battery of forms, and underwent medical tests, including an ECG. I listened as intake specialists laid out the details of the study: the prospect of healing after multiple sessions with two therapists, three MDMA “journeys”—or placebo journeys, as the case may be, since half the participants would be relegated to those—and additional “integrative” sessions during which I would make sense of what “the medicine” and the conversations had revealed to me.
Ultimately, I was passed over for the study—a rejection that was more crushing than I would have predicted. It sent me on a search through the elaborate psychedelic therapeutic underground. The licensed therapists I found who were psychedelic-friendly were careful to say that they did not provide the substances themselves; the patient would have to procure them. By contrast, the facilitators who dwelled in the gray market of this treatment were very open about their ability to source and dispense these substances; none, however, were trained therapists or psychiatrists. That left group treatment settings as the remaining option, but this remedy—which involved sleeping in a room with strangers of both sexes when one’s defenses were drastically reduced—seemed fraught with emotional and even physical risks.
A growing sense of urgency made me want to learn more, which is why I took to interviewing or simply questioning anyone who crossed my path who had what I perceived to be expertise in the therapeutic use of psychedelics. But the more I learned, the further treatment seemed to slip from my grasp. When could I get the ecstasy that was the potential cure for my night terrors?

My research taught me that I was not the only person struggling with access. Last June in Denver, MAPS drew 12,000 people to its fourth annual Psychedelic Science conference—the largest gathering of its kind ever. Many attendees were concerned with the access question. A sign hanging next to the booth of the Psychedelic Access Fund, a New York City–based nonprofit that describes itself as offering “psychedelic access for underserved communities,” noted that the cost of six ketamine infusions ranges “between $2,000 and $6,000.” And during the final session’s keynote speech, titled “Reflections on Psychedelic Science 2023,” a group of Indigenous activists interrupted the speaker, MAPS founder Rick Doblin, to protest the lack of Indigenous representation at the conference. “Can we get your attention? This is not a revolutionary movement if you are leaving people out of the conversation,” one of the activists shouted.
When I spoke with Doblin over Zoom several months later, I asked him what he thought of the demonstration. “Indigenous people are coming from incredible pain and suffering,” he said. Nonetheless, he defended his organization’s record, saying that MAPS had tried to make the event welcoming and accessible to Indigenous attendees, spending $100,000 on transportation, lodging, and other expenses while also giving out 234 scholarships to people who self-identified as indigenous. He also touted the work that MAPS has been doing to try to make the psychedelic therapy movement more diverse and equitable. “We are receptive, not the evil oil companies,” he said.
Popular
“swipe left below to view more authors”Swipe →Even so, the protest at the Denver conference highlighted a central paradox within the field: A number of these drugs were discovered and used for centuries by Indigenous and West African peoples, but many of their descendants now have limited access to them. And the high price of obtaining these drugs, I soon found, has sent a number of people down the DIY route.
One Denver resident I spoke with, who asked to go by the name Nellie for this piece, had started a meetup group for what she calls “psychedelic support.” Nellie is an alternative health practitioner whose income from her part-time work puts her close to the poverty line, making it impossible for her to afford $400 ayahuasca group trips or three hours of her therapist’s time for a ketamine trip. She feels that these therapies would help her address the PTSD she developed from growing up in an abusive household. “I am working-class—I have an associate degree and am studying to be an herbalist—but I also need to go on psilocybin journeys as it’s good for the trauma, which I have plenty of,” Nellie said.
When Nellie and the other members of her DIY group meet, they each take four grams of mushrooms. Nellie doesn’t deny that there are dangers involved in taking psychedelics with a group of other people and no trained facilitators. “I do feel safer with a facilitator in the room,” she acknowledged, recalling the stress of a journey during which one member melted down in “grief and pain” while everyone else was high themselves. But for now, that’s all she can do.
Another person I spoke with, Evan, 24, grew up poor in a family of Mexican descent and views mushrooms as the reason he swerved away from the life of physical labor that he believed he had been “programmed to accept.” Today, Evan works as a mental health counselor but earns just “25K a year,” he said. So he grows his own psilocybin mushrooms and then consumes some himself and distributes the rest for free to low-income people. “Some people spend their evenings watching TV or going to the bar,” he said. “I grow mushrooms in clean closets.”
Leaders in the psychedelic healing industry are aware that they have an inequity problem on their hands—aware enough, at least, to include shout-outs to “access” and “inclusion” in their promotional materials. “We’re working to ensure our therapies are broadly and equitably accessible to all who might be helped by them,” reads a blurb on the website of Compass Pathways, a biotech company backed by Peter Thiel.
But as welcome as awareness is, the current corporate efforts at inclusion are mostly gestural—and they certainly haven’t lowered prices. So what can actually be done to nip psychedelic inequality in the spore?
When I asked Doblin how he imagined the future of psychedelic-assisted therapy unfolding, he responded with a flurry of predictions that seemed to hover somewhere between rigorous action plan and wishful fantasy. As a first step, he said, the FDA should approve MDMA-assisted treatment—one of the therapies that MAPS has been most focused on—and he anticipated this could happen as early as the end of 2024. This would open the door to the possibility of insurance coverage as well as patient assistance programs for those who can’t afford the treatments. From there, he said, he envisions MAPS and other groups getting to work training therapists—as many as 25,000 by 2030—in administering MDMA safely and effectively.
Doblin was also optimistic about the fate of other treatments. “Psilocybin will be approved. There will be an advancing of research—and a continued undermining of confidence in and support of the drug war,” he predicted.
If all this has echoes of utopia, it does get one crucial thing right: For there to be any hope of increasing access to these therapies, there must be FDA approval followed by widespread insurance coverage. Without the former, there can’t be the latter; and without the latter, there’s little hope that any of these treatments will ever be affordable.
That said, this is the United States, a country famous for its broken health insurance system, which means that even if advocates score widespread insurance coverage, psychedelic therapies will simply have achieved the same dreary status of most existing therapies. As Donald Moynihan, a professor at the McCourt School of Public Policy at Georgetown University, told me, there’s a big gap “between health services being theoretically available and actually accessible.”
The first hurdle is health insurance itself, which is inadequate in many cases and nonexistent for more than 8 percent of the population. Then there’s the question of what Moynihan calls “administrative burdens,” which include the time an individual has to spend tracking down a new resource like therapeutic psychedelics. That, he said, is often “a significant barrier.” In addition, for “unconventional new treatments,” there are “learning costs”—the time and savvy it takes for people to find out about them.
To address these fundamental challenges, advocates have suggested expanding the use of psychedelics on religious grounds as a framework to increase access. Today, only a few religious groups can use only a small number of psychoactive substances under the 1993 Religious Freedom Restoration Act. If religious use could be expanded, then more people would have more access. (Critics have raised concerns, however, about the potential for exploitation in certain religious settings, such as in cults.)
Advocates have also argued that access could be improved through both decriminalization and legalization (with regulation) of psychedelics. Kevin Balktick, who founded Horizons, a psychedelics media and education organization, explains the difference between decriminalization and legalization this way: “Decriminalization largely just takes away handcuffs” for personal possession, he told Lucid News, while legalization is broader, allowing “people to offer products and services to start, fund and operate businesses, and to really build an ecosystem.”
These last two steps are important ones, and they would certainly expand access. Even so, critics warn, they would also risk creating a two-tiered system in which rich people have access to trained therapists while everyone else has “trip sitters” at best. Or, put another way, a system that relies on religious and recreational access to solve its inequality problems risks leaving out one of the most essential parts of psychedelic-assisted therapy: the therapy itself.
This, in fact, is not all that different from where Katy, the Colorado mother seeking help for her addiction, finds herself now. When I last spoke with her, she told me she had begun to explore DIY psychedelic therapy, taking home “a bunch of mushrooms” from a visit to a cultivator she had met at a local psychedelics club. Katy measured them out on a scale she’d purchased, swallowed them down, closed her eyes, and saw colors. She did not, however, have anything close to the transformative experience she’d had at her professionally facilitated psilocybin treatments. But she felt she didn’t have any other choice; she can’t keep putting sessions on credit cards she can’t pay off.
So what can Katy do now? The financial impossibility of getting the help she needs is the ultimate bitter pill—and it will keep these treatments out of reach for Katy and others like her unless supports are put in place. Without this treatment, she asked, can she stay better?
Thank you for reading The Nation
We hope you enjoyed the story you just read, just one of the many incisive, deeply-reported articles we publish daily. Now more than ever, we need fearless journalism that shifts the needle on important issues, uncovers malfeasance and corruption, and uplifts voices and perspectives that often go unheard in mainstream media.
Throughout this critical election year and a time of media austerity and renewed campus activism and rising labor organizing, independent journalism that gets to the heart of the matter is more critical than ever before. Donate right now and help us hold the powerful accountable, shine a light on issues that would otherwise be swept under the rug, and build a more just and equitable future.
For nearly 160 years, The Nation has stood for truth, justice, and moral clarity. As a reader-supported publication, we are not beholden to the whims of advertisers or a corporate owner. But it does take financial resources to report on stories that may take weeks or months to properly investigate, thoroughly edit and fact-check articles, and get our stories into the hands of readers.
Donate today and stand with us for a better future. Thank you for being a supporter of independent journalism.
More from The Nation
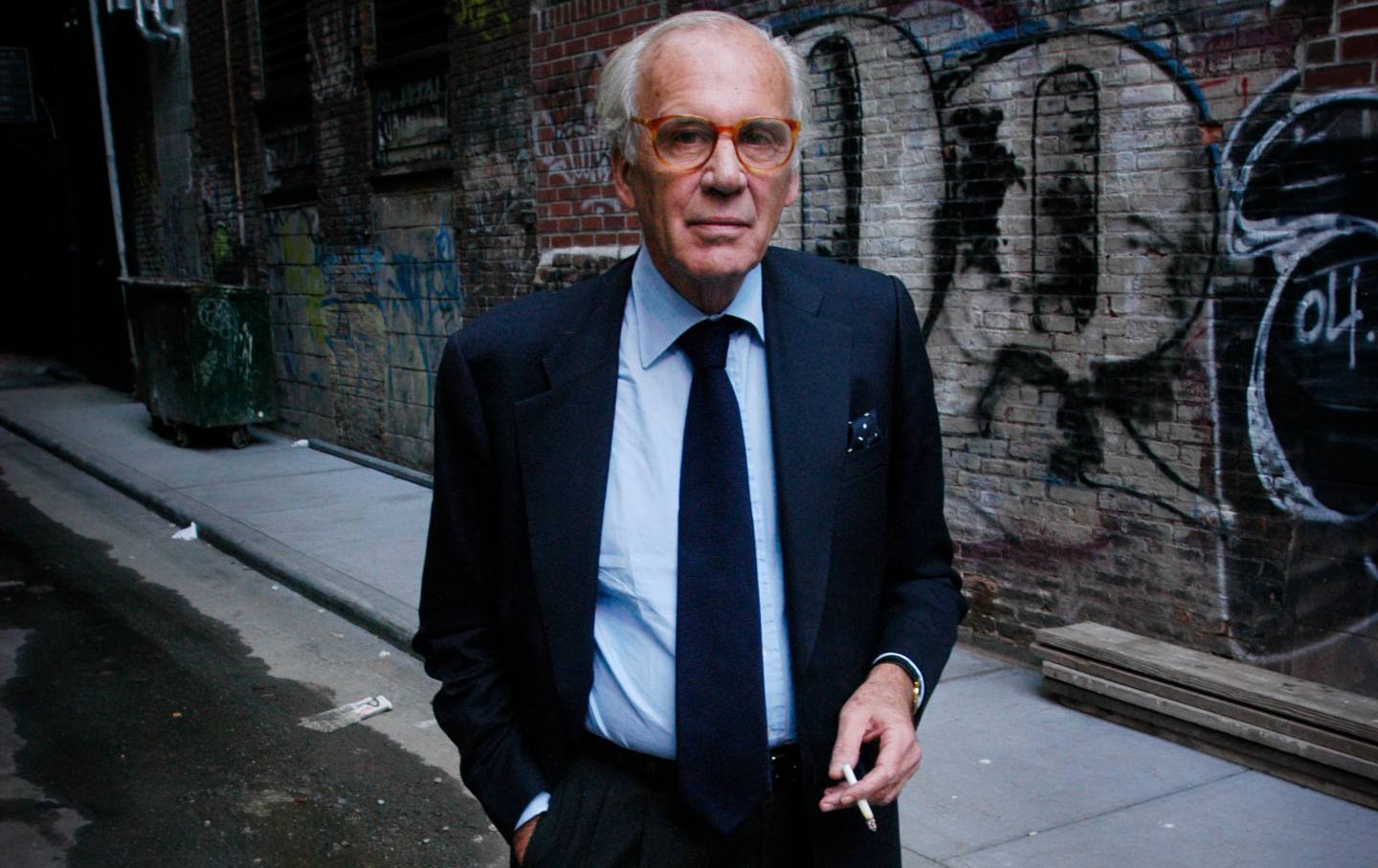
Lewis Lapham Salvaged From History What Was Useful, Beautiful, and True Lewis Lapham Salvaged From History What Was Useful, Beautiful, and True
Writer Lewis H. Lapham, longtime editor of Harper’s Magazine and the founder of Lapham’s Quarterly, died in Rome. He was 89.

The Paris Olympics Are Kicking Off With Protests The Paris Olympics Are Kicking Off With Protests
“The Olympic Games are profoundly disrupting the lives of French people,” the protesters wrote in a joint statement.“The question then arises: Who benefits from the Games?”

Biden Said Rent Cap. Here’s What Tenant Organizers Say Must Happen Next. Biden Said Rent Cap. Here’s What Tenant Organizers Say Must Happen Next.
The president called on Congress to act, but he could enact a rent stabilization policy with a stroke of his pen. Tenant leaders say they will keep organizing until it happens.

Why There Are No Trans Women Competing at the Paris Games Why There Are No Trans Women Competing at the Paris Games
There are at least two trans nonbinary athletes—Quinn and Nikki Hiltz—and they’re impossible not to cheer for.

The Appalling Social Cleansing of Olympic Paris The Appalling Social Cleansing of Olympic Paris
In the last year, an estimated 12,500 vulnerable Paris residents were forced from their homes.

At My High School, the Library Is for Everything but Books At My High School, the Library Is for Everything but Books
The administration has rebranded our library as a communal space for doing almost everything except reading.