Puerto Rico’s Unnatural Disaster
The island’s health system is on its knees. Doctors are fleeing in droves. And the crisis is hurting children most of all.
The Unnatural Disaster Threatening Puerto Rico’s Children
The island’s health system is on its knees. Doctors are fleeing in droves. And the crisis is hurting kids most of all.

San Juan, Puerto Rico—Yarelys Díaz Rivera was desperate. Her young daughter, Isabella, was gravely ill. What had begun as seemingly mild stomach problems had turned into a life-threatening heart condition. And Díaz Rivera, a 39-year-old mother from the rural and mountainous Puerto Rican town of Corozal, couldn’t find the healthcare she needed on the island.
Isabella was already starting from behind. The doctors had misdiagnosed her for a month before they finally figured out that she had an enlarged heart and needed a heart transplant. Others refused to take Díaz Rivera’s insurance.
After Isabella spent another month in Centro Médico, Puerto Rico’s largest hospital, it became clear that she would need surgery that was simply not available on the island, which has just one pediatric heart surgeon for a population of nearly 3.3 million people. Instead, Díaz Rivera would have to take her daughter to the mainland United States.
This was easier said than done. Before the family could go, they needed to get approval for the surgery from their insurance company, First Medical. Instead, First Medical slowed the process to a crawl. “I had to explain a thousand and one times to the company why I needed approval for Isabella immediately,” Díaz Rivera told The Nation.
“The hospital had to call First Medical directly. The air ambulance company had to call First Medical directly to get approval,” she continued. “Having health insurance in Puerto Rico felt just the same as not having insurance at all.”
Eventually, First Medical decided it would cover only about 15 percent of the roughly $350,000 cost of Isabella’s treatment. It refused to cover the rest because the procedure would take place outside of Puerto Rico, leaving Díaz Rivera and her family on the hook for about $300,000. (She eventually qualified for Pennsylvania Medicaid, which covered the rest.)
Díaz Rivera quit her job working in education in April 2023 and traveled with Isabella over 1,700 miles to the UPMC Children’s Hospital of Pittsburgh, which has a special relationship with Centro Médico. Isabella was now 17 months old. Díaz Rivera’s husband and their 12-year-old twins visited them numerous times, but they couldn’t stay in Pittsburgh permanently.
Between the massive bills, her daughter’s life-threatening condition, her separation from the rest of her family, and the knowledge that her other children were growing up on an island threatened by natural disasters, power outages, and economic crises, Díaz Rivera had a mountain of burdens to bear.
“It’s really hard to go through all of this,” she said. “I had to leave the rest of my family behind and practically move to a new country. My husband has to keep working because we still have to pay the bills, and those definitely don’t stop in Puerto Rico. I have a lot of support from my family, but it’s such a hard situation.”
Díaz Rivera’s story is far from unique. Isabella wasn’t even the only baby from Puerto Rico being treated at the UPMC Children’s Hospital—Díaz Rivera met another couple who had to leave the island to get care for their 3-month-old son, and whose insurance company would agree to cover only part of the procedure. That family faced an initial bill of around $400,000, which was eventually covered by Medicaid. Both families, along with scores of others back in Puerto Rico, were dealing with the fallout of the severe healthcare crisis that has gripped the island for the past 15 years.
US healthcare is defined by the greed and inequality that its patients must battle, but Puerto Rico’s calamity is unique. Thanks to a combination of colonial neglect, a disastrous legacy of privatization that has given health insurance companies outsize control, and a series of devastating austerity measures in recent years, it’s not just patients who are feeling the impact; it’s also the people who are supposed to look after them. Puerto Rico has seen a mass exodus of doctors that has left it struggling to provide even the most basic level of care. And no medical specialty has been affected more than pediatrics, leaving families like Díaz Rivera’s with gut-wrenching choices to make.
Puerto Rico’s healthcare system remains notably more threadbare than that of the rest of the United States. As citizens of a US territory under colonial administration, Puerto Ricans pay Social Security and Medicare taxes just like other US residents, but they receive only around $5,119 per capita in annual federal healthcare funding, compared with $14,170 per capita at the national level. In part, this is because the federal government typically uses less generous methods to determine Puerto Rico’s funding levels than it does for the 50 states. This imbalance is pronounced in a territory where more than 40 percent of the population lives below the poverty line, a figure that dwarfs that of even the poorest states in the US, such as Mississippi’s 19 percent poverty rate.
Puerto Ricans have been eligible for coverage under Medicaid since its inception in the 1960s. At the time, the island’s healthcare system—the management of which devolved to the Puerto Rican government—bore the hallmarks of a socialized-medicine model unique within the United States.
In 1961, two-thirds of Puerto Ricans received free healthcare, and 63 percent of hospitals were government facilities. Healthcare providers, including doctors, were categorized as government employees, and their services were provided in publicly funded clinics and hospitals all over the island. Rural areas, which typically lacked good transportation to the capital, San Juan, benefited the most from this system.
However, rising healthcare costs and the spread of neoliberal ideology weakened support for the more socialized model, and in 1993, then-Governor Pedro Rosselló introduced “La Reforma,” a sweeping healthcare overhaul that privatized nearly every public hospital and clinic in Puerto Rico.
La Reforma was pitched as a way to boost doctors’ wages and incentivize them to continue to provide quality care to the publicly insured. But three decades on, the opposite has happened: Rather than strengthening its healthcare system, Puerto Rico has seen a staggering loss of its medical professionals. The Center for a New Economy, a think tank in Puerto Rico, estimated last year that the island may have lost nearly half of its doctors in just over a decade; more than 8,000 are thought to have left since 2009. The reasons are clear: The Puerto Rican healthcare system is buckling under the effects of severe disinvestment, and its professional workforce is underpaid.
Given these circumstances, doctors not only find themselves in dire financial straits personally, but they are also unable to provide adequate care for their patients. Pediatricians are particularly affected; unlike cardiologists, dentists, and other doctors who benefit from Medicare’s coverage of seniors, they are penalized by a system biased toward coverage for an aging society. Pediatricians in particular cite low reimbursement rates from health insurers as their main reason for departing the island.
The number of pediatricians on the island has dropped more than 25 percent over the past decade, from 700 to 500, leaders from Puerto Rico’s top pediatric associations announced during a press conference convened last summer to address the crisis facing their specialty. An alarming 75 percent of the country’s pediatricians are over the age of 50 and approaching retirement. Medical-school graduates are leaving the island en masse for better opportunities in the United States, where the average yearly income for pediatricians is nearly double what it is in Puerto Rico.

This disaster is part of a larger brain drain brought on by Puerto Rico’s decision to undergo what proved to be the largest municipal bankruptcy in US history. Oversight of the territory’s finances rests with an unelected seven-member board appointed by Congress. This body has imposed brutal austerity measures on Puerto Ricans to fulfill the public-debt obligations to bondholders, causing the cost of basic services to spike while government assistance was slashed. Students enrolling in the cash-strapped public university face tuition hikes amid multimillion-dollar budget cuts, resulting in reduced course options and crumbling infrastructure. And even if the students do graduate, they often seek opportunities elsewhere, leaving the island short of professionals in every field and generations of all ages bereft of adult family members.
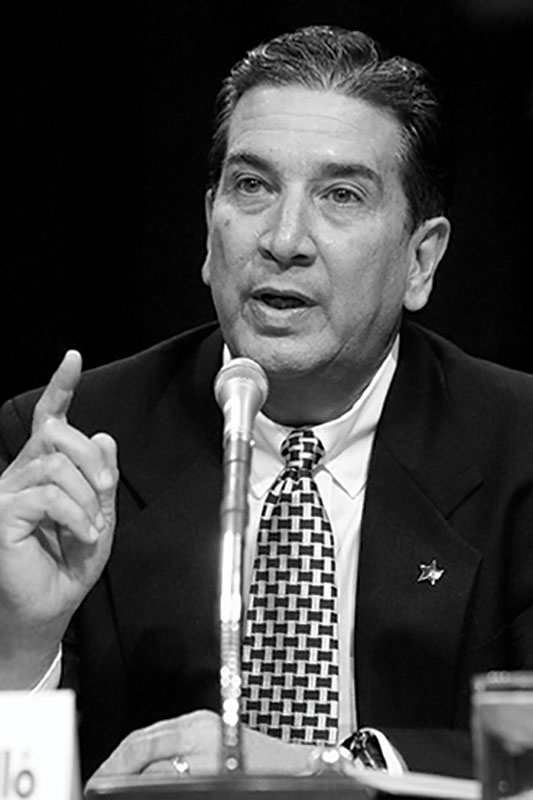
Facing Puerto Rico’s many hurdles, Daniel Vélez Reyes bought a one-way ticket to Arizona in 2012. At the time, he was one of just three pediatric heart surgeons on the island. Now there is only one.
Vélez Reyes, 55, had dedicated six years to Centro Médico in San Juan, but he tired of the relentless delays in insurance reimbursements. In addition to waits of up to three months for payment, his claims were frequently rejected by insurers because they “lacked documentation.” He often resubmitted them himself in exactly the same way, and the claims would be approved.
Vélez Reyes eventually reached a breaking point and moved to Phoenix, where he now works at the city’s children’s hospital.
“In the 12 years I’ve been here [in the US], I’ve never experienced this tendency” for companies to reject so many claims, he said. “I don’t see myself coming back to Puerto Rico for any reason. But I’m still trying to look for ways that I can help alleviate what’s on the horizon, which is a total lack of cardiovascular surgeons in Puerto Rico—especially pediatric.”

The medical brain drain leaves doctors in all fields worried about how patients’ health will be affected as the years go by.
Norma Devarie Díaz is a cardiologist and the president of Coalición Nueva Visión de Salud (New Vision for Health Coalition), a collective of healthcare professionals, patient associations, and students pushing for policy reforms to elevate the quality of care for all Puerto Ricans. “If a child doesn’t receive the right care,” she said, “I’m going to be getting patients with diabetes, high blood pressure, and prone to heart attacks. That’s why it’s important to have up-to-date primary care, but prevention here doesn’t exist.”
These days, Puerto Rico provides Children’s Health Insurance Program coverage to children under the age of 19, basing eligibility on the local poverty level rather than the federal level. As of August 2021, Puerto Rico had enrolled 1.5 million people—about 46 percent of the population—in Medicaid and CHIP. (Twenty-seven percent are on Medicare, and 31 percent have private insurance.)
But funding doesn’t mean much if there are no doctors to go to. Ask anyone living on the island about getting an appointment, and they will tell you about the six-to-12-month wait to see a specialist for a nonurgent case.
The island’s Medicaid program, the Government Health Plan, also known as Vital, has been the target of strong criticism over the years. Although it’s a public program, it is run by four major private health insurance companies: First Medical, MMM, Menonita, and Triple-S. The system has been faulty, at the very least, with reimbursement rates that are vastly lower than in the states.
In 2023, the four big insurance companies faced fines totaling $300 million for failing to pay doctors the minimum rates established for medical services during the first half of the year. And the program is no stranger to corruption: In 2019, the former executive director of Puerto Rico’s Health Insurance Administration, Ángela Ávila-Marrero, was indicted for her role in a scheme to steal federal Medicaid dollars through a corrupt bidding process with private contractors. Healthcare professionals have gone so far as to call the system a “health cartel.”
“It breaks my heart to think of all the children who are still stuck in hospitals in Puerto Rico, waiting for care, because of health insurance companies,” said Nora Maldonado Carrión, a 63-year-old whose grandchild was in the same Pittsburgh hospital as Diaz Rivera’s daughter. “Where are all their profits going? We’re left without any doctors.”
Puerto Rico’s Department of Health and its Health Insurance Administration did not respond to multiple requests for comment from The Nation.
For doctors treating adults, the strategy for making a living in this situation is a no-brainer: prioritize elderly patients covered by Medicare, which offers higher payments than Medicaid, compensating for the shortfall. But pediatricians don’t have that option.
Gerardo Tosca Claudio, a pediatrician in San Juan and the president of the Puerto Rican Society of Pediatrics, noted that children’s doctors receive $25 to $38 for a new-patient visit and $18 to $25 for follow-up visits. By contrast, doctors on the US mainland often receive more than $100 for new-patient visits. The 55-year-old said he hasn’t seen the rates from private insurance companies change in more than 20 years. “It’s frustrating—I haven’t seen my reimbursement rates go up in decades,” he said.
Payment delays, which can sometimes continue for months, also add fuel to the fire. Relying solely on Medicaid isn’t feasible for doctors in Puerto Rico. Inflation, which spikes the cost of living, and chronic power disruptions, which make it a struggle simply to keep a medical practice functioning from day to day, compound the challenge.
The situation is particularly worrisome for children. Early childhood care is fundamental for establishing good health and preventing poor medical outcomes later in life. Any gap in that care puts children at risk.
Predictably, Puerto Rico’s insurance companies insist that they’re not at fault. José Novoa Loyola is a cardiologist as well as the chief medical officer of Triple-S at the Medicaid and Medicare Advantage Products Association of Puerto Rico, a coalition representing the island’s major health insurance companies. He told The Nation that doctors receive lower payments in Puerto Rico compared with those in the states because the premiums for customers are also lower, not because the insurance companies are hoarding wealth. And though he acknowledged that the pediatrician shortage is “a particular problem we have to deal with and give priority to,” Novoa Loyola defended the system he represents. “In a capitalist system, you have a right to profit,” he said. “Part of the health system is business.”

The inadequacy of Puerto Rico’s healthcare funding is felt most acutely during economic downturns and natural disasters such as Hurricane María in 2017, which struck just months after the island’s bankruptcy declaration. The Category 4 hurricane was the strongest storm to hit Puerto Rico in almost a century; a Harvard study estimated the death toll at 4,645 people.
After María, the federal government waived or modified certain Medicare, Medicaid, and CHIP requirements to provide immediate relief to those affected by the hurricane, but healthcare providers believe the practice of medicine shouldn’t depend on the arbitrariness of natural disasters. The chaotic medical situation in the aftermath of María, coupled with the power outages, prompted numerous doctors to seek work elsewhere. Three months after the storm, lawmakers estimated that 10 doctors were leaving the island each day. But even before María, pediatricians were ringing alarm bells. The impact is felt most severely by people outside the San Juan metropolitan area, as is often the case when disaster strikes in Puerto Rico.
Power outages remain a paramount concern all over the island. Viewers of local television in Puerto Rico are no strangers to commercials touting solar panels as a remedy for the perpetual power disruptions, joining the sometimes cringeworthy health insurance commercials tailored to older people.
Popular
“swipe left below to view more authors”Swipe →The fluctuations in electricity, along with rising utility costs, have caused many pediatricians to stop providing vaccines that require refrigeration at their practices. As a result, parents are now turning to pharmacies and vaccination centers to keep their children’s immunizations current, but this alternative comes with a sacrifice.
“When a patient gets vaccinated with a pediatrician, the doctor performs a screening, monitoring a child’s developmental milestones and letting parents know what they should be looking out for,” said Nilka de Jesús González, the president of the Puerto Rico chapter of the American Academy of Pediatrics. “All this is lost when vaccination visits don’t happen.”
That’s why doctors like Norma Devarie Díaz are organizing to promote a new system that prioritizes health over profit. In May 2023, members of Coalición Nueva Visión de Salud demonstrated with signs that read “Health is not an industry because patients are not merchandise” and “More health, less lies” in front of the Capitol in San Juan.
Some health experts, like Heriberto Marín Centeno, a professor at the Graduate School of Public Health at the University of Puerto Rico, advocate a more profound overhaul: creating a national health insurance system that would offer universal healthcare. Such a model would also address the island’s uninsured, estimated by Marín Centeno to be about 5.5 percent of the population. “We have an oligopolistic market where health professionals are trapped and unable to negotiate their rates,” he said. “Health insurance companies are making themselves rich thanks to this system. This is why we’re proposing universal healthcare, where health insurance companies are not the main entity in charge of managing public funds.”
Sometimes, all of the elements in Puerto Rico’s healthcare crisis—the lack of doctors, the lack of adequate care for children, the lack of facilities and money and equipment—coalesce in particularly heartbreaking ways.
Ever since Hurricane María destroyed the only medical center in Vieques, an islet 10 miles away from the main island, it has lacked a functioning hospital. The 8,000 people living in Vieques usually have to take a ferry to the main island for medical care. The trip takes 30 minutes to an hour—time that could mean the difference between life and death in an emergency. Many residents attest that whatever challenges Puerto Ricans face, Viequenses take the hit tenfold.
In January 2020, a 13-year-old girl in Vieques named Jaideliz Moreno Ventura went into convulsions. Her family took her to a local clinic, but it didn’t have a functioning respirator to give her the oxygen she needed. Jaideliz died in an air ambulance on the way to the main island.
Recently, I accompanied Jessica Ventura Pérez, Jaideliz’s mother, to her daughter’s grave. It was covered in pink flowers and bindweeds, and a teddy bear hung over a flat arch overlooking the Caribbean greenery.
The gravestone lacks any words or numbers. Even Jaideliz’s name is not there, because for Ventura Pérez, those things are hollow compared to what she has lost. She has channeled her grief into a lawsuit against the Puerto Rican government for violations of her daughter’s human and civil rights. (The case is still pending.)
Ventura Pérez comes from a long line of fighters. Until it withdrew 20 years ago amid massive protests, the US Navy used Vieques as a firing range and testing ground for munitions. Ventura Pérez’s father and grandfather had joined the movement to expel the Navy after a military plane accidentally bombed a civilian watchtower, killing a security guard and wounding four others.
Ventura Pérez’s fight and that of her father and grandfather are the same, really, as is the fight to keep more pediatricians on the island. It’s a fight against colonial rule, against a system that’s oblivious to Puerto Rico’s most vulnerable people, against governments and institutions defined by neglect and mismanagement. It’s the fight to make Puerto Rico a place where a mother like Yarelys Díaz Rivera doesn’t have to upend her entire world to get her child lifesaving surgery, or where a mother like Jessica Ventura Pérez doesn’t have to bury her child because nobody had bothered to construct a hospital where one was needed.
“Whatever happens, even if they build a new hospital, my daughter isn’t coming back,” Ventura Pérez said. “But I can prevent another death of a loved one from happening.”
Her conviction was palpable, but her voice started to crack when she looked down at her chest, where a locket with her daughter’s picture rested.
Thank you for reading The Nation
We hope you enjoyed the story you just read, just one of the many incisive, deeply-reported articles we publish daily. Now more than ever, we need fearless journalism that shifts the needle on important issues, uncovers malfeasance and corruption, and uplifts voices and perspectives that often go unheard in mainstream media.
Throughout this critical election year and a time of media austerity and renewed campus activism and rising labor organizing, independent journalism that gets to the heart of the matter is more critical than ever before. Donate right now and help us hold the powerful accountable, shine a light on issues that would otherwise be swept under the rug, and build a more just and equitable future.
For nearly 160 years, The Nation has stood for truth, justice, and moral clarity. As a reader-supported publication, we are not beholden to the whims of advertisers or a corporate owner. But it does take financial resources to report on stories that may take weeks or months to properly investigate, thoroughly edit and fact-check articles, and get our stories into the hands of readers.
Donate today and stand with us for a better future. Thank you for being a supporter of independent journalism.
More from The Nation
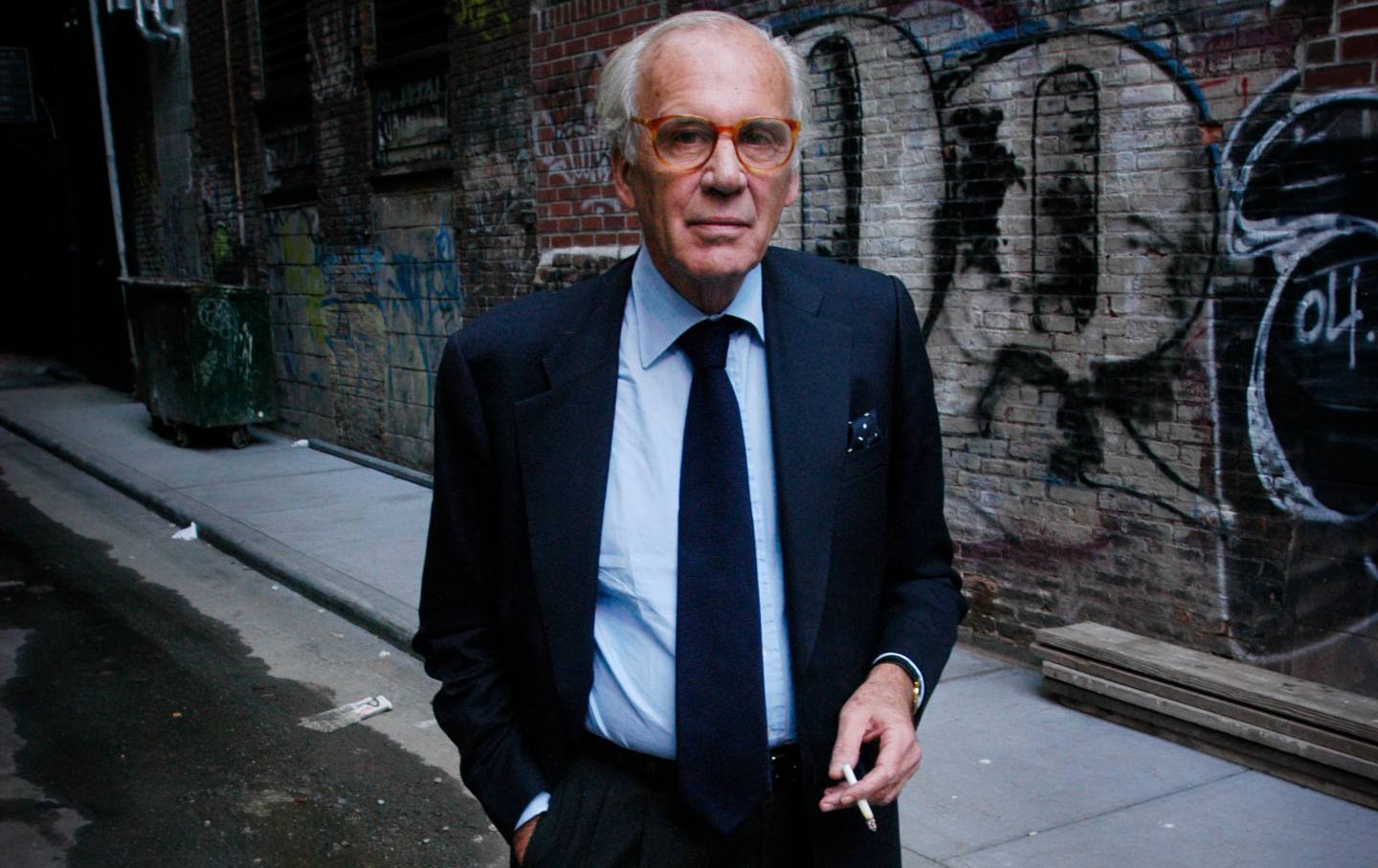
Lewis Lapham Salvaged From History What Was Useful, Beautiful, and True Lewis Lapham Salvaged From History What Was Useful, Beautiful, and True
Writer Lewis H. Lapham, longtime editor of Harper’s Magazine and the founder of Lapham’s Quarterly, died in Rome. He was 89.

The Paris Olympics Are Kicking Off With Protests The Paris Olympics Are Kicking Off With Protests
“The Olympic Games are profoundly disrupting the lives of French people,” the protesters wrote in a joint statement.“The question then arises: Who benefits from the Games?”

Biden Said Rent Cap. Here’s What Tenant Organizers Say Must Happen Next. Biden Said Rent Cap. Here’s What Tenant Organizers Say Must Happen Next.
The president called on Congress to act, but he could enact a rent stabilization policy with a stroke of his pen. Tenant leaders say they will keep organizing until it happens.

Why There Are No Trans Women Competing at the Paris Games Why There Are No Trans Women Competing at the Paris Games
There are at least two trans nonbinary athletes—Quinn and Nikki Hiltz—and they’re impossible not to cheer for.

The Appalling Social Cleansing of Olympic Paris The Appalling Social Cleansing of Olympic Paris
In the last year, an estimated 12,500 vulnerable Paris residents were forced from their homes.

At My High School, the Library Is for Everything but Books At My High School, the Library Is for Everything but Books
The administration has rebranded our library as a communal space for doing almost everything except reading.