Doctors Are Employees Now. It’s Time for Us to Unionize.
Organizing doesn’t just benefit our own working conditions. It can improve the lives of patients, too.
Medicine in America is a dying profession. A profession, according to the mathematician and polymath Charles Sanders Peirce, is a “community of the competent,” a group of experts entrusted by society to manage their own affairs. From the rites of initiation, to the regulations governing everyday practice of their craft, professionals are given significant autonomy in their areas of expertise. When medicine was a field made up of private practitioners who self-governed through medical societies, Peirce’s definition was a reasonable approximation of the state of the field. But that era is over.
Between 1983 and 2014, the percentage of physicians practicing alone in the United States declined from 41 percent to 17 percent. By 2022, 74 percent of physicians were employed by hospitals, health systems, and other corporate entities, including private equity firms and health insurers. The image of the independent physician with a shingle outside the door and a satchel of instruments for home visits is a comforting bit of nostalgia, but it is not, for most of us working in the US, a present reality. We are, more and more, employees of large entities run not by physicians but by financial executives with no role in or even experience with the care of the sick. This lack of connection to direct patient care fosters a skewed understanding of patients as “clients,” “consumers,” or “customers,” rather than vulnerable people who have allowed us to enter into a sacred trust.
The decade-long process of medical school and residency has long been ruled by hierarchical relationships and vulnerability to the whims of our superiors. Now, that period of professional adolescence continues even after our training, as early in our careers we are dependent on our employers if we want to pay back six-figure medical school debt.
I learned about this vulnerability in 2019. After hearing patients in the emergency department where I worked worry aloud about the cost of the care they were receiving and reading about lawsuits against patients in debt filed by hospitals around the country, I went to my county courthouse to find out how hospitals in my area dealt with patients in debt. There, I found that my very own hospital system was filing suits against single mothers, disabled people, and other low-income patients who could not afford their hospital bills. If they did not agree to onerous payment plans, part of their wages were withheld and sent instead to the hospital. When I wrote about the practice for a blog called UpriseRI, I immediately received a call from hospital administrators demanding that I retract the piece and follow the chain of command for complaints in the future. When I refused to take the piece down, I was made to sit through a meeting with a hospital administrator who told me, like a chagrined father, how disappointed he was. A few weeks later, the hospital dropped its remaining lawsuits against patients and severed its relationship with its debt collection agency.
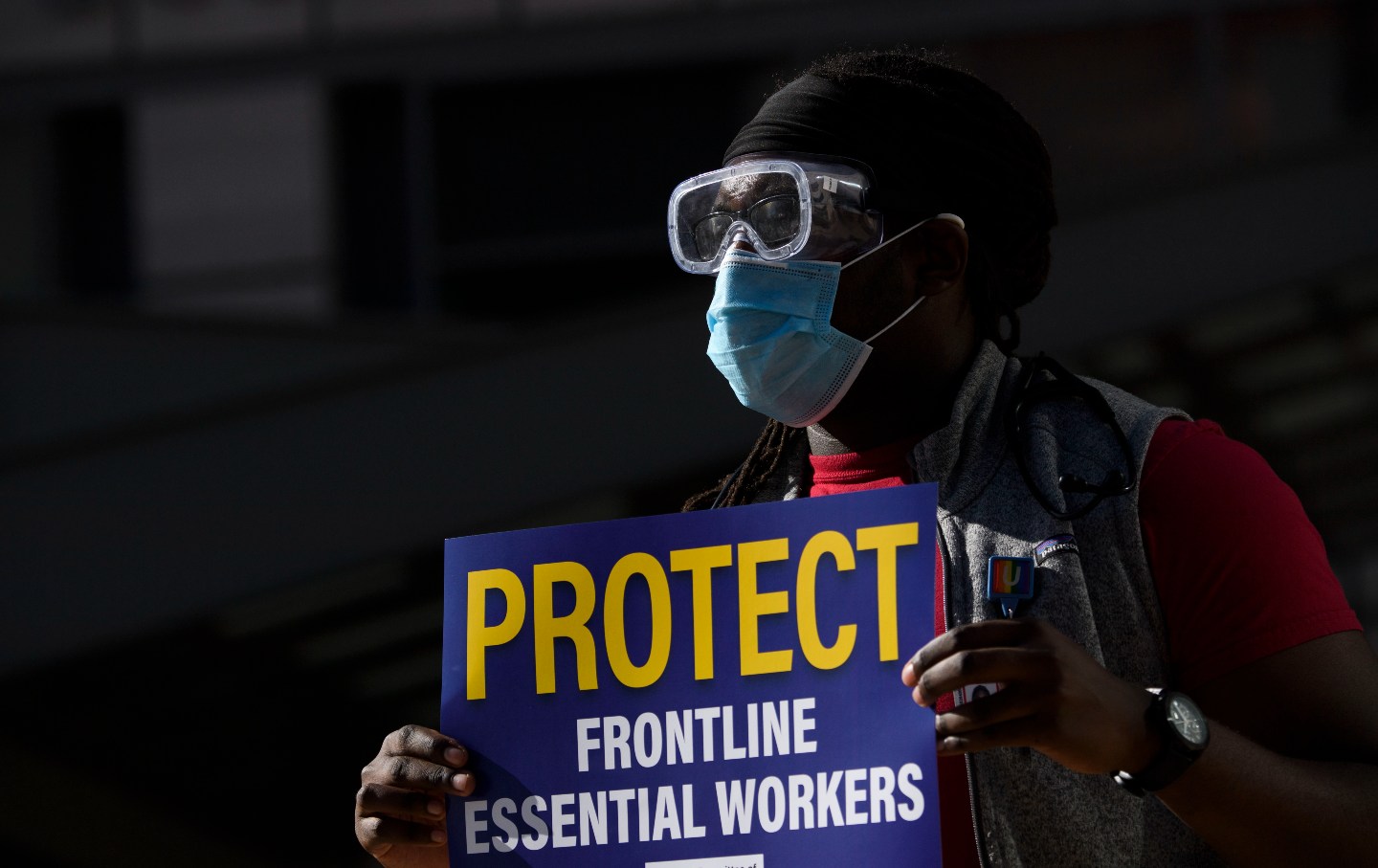
When the Covid pandemic hit the United States, medical professionals everywhere in the country would learn about the loss of professional independence. We used disposable masks for an entire shift, then placed them in paper bags to be reused day after day. This was, in the words of the Centers for Disease Control, a practice “not commensurate with US standards of care,” but instead of sounding the alarm and increasing production, President Trump claimed that the problem was health workers’ stealing masks. Clinicians were making wrenching decisions based on shortages of ventilators and other breathing machines. When doctors and nurses spoke out about these shortages, calling on our government to increase capacity, they were reprimanded by their own hospital administrators for speaking critically about working conditions, and some physicians even lost their jobs. The nation’s largest medical societies, including the American Medical Association, responded with statements affirming physicians’ right to advocate for themselves, their colleagues, and their patients, but it was clear that the balance of power had shifted decisively away from professional organizations.
Over the past few decades, physicians have transformed from independent professionals to employees of sprawling, hierarchical organizations. Part of the appeal of medicine for many of us was its promise to not only allow us to harness our scientific expertise to help patients, and earn a comfortable living doing so, but also to offer us some measure of autonomy to make the decisions we think best for our patients.
To be sure, the professional autonomy of physicians has not always worked for the benefit of society at large. At the height of its power in the mid-20th century, the American Medical Association used its political might to fight the passage of national health insurance. Yet our present health care system—ruled by rentiers like health insurance companies, pharmacy benefit managers, private equity companies and debt buyers, and largely unregulated profit-maximizers like pharmaceutical companies and for-profit health care facilities—is hardly an improvement.
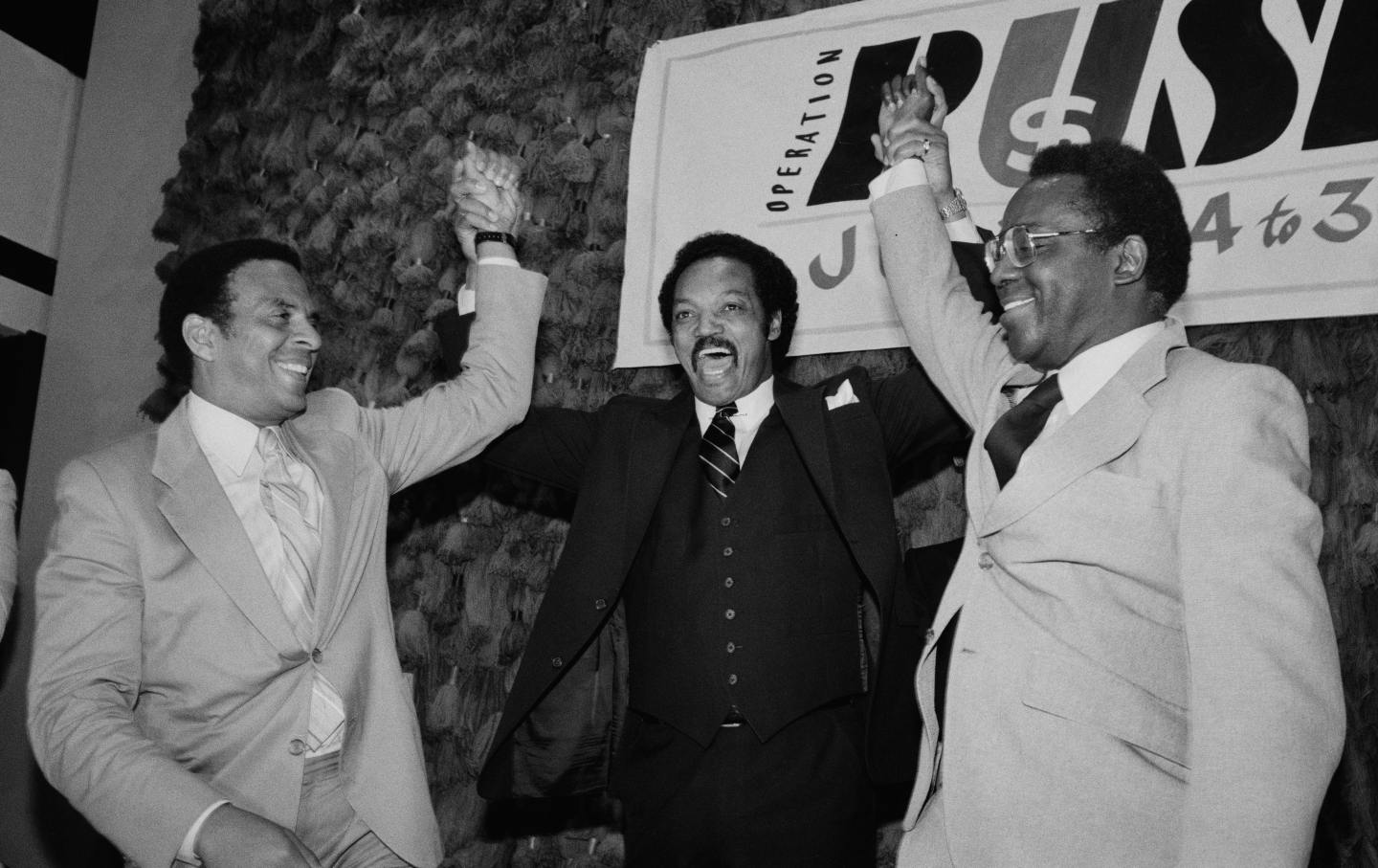
The reality is that the days of the independent physician will never return in America. Instead, doctors must own our roles as employees of large systems in order to begin more effective organizing. Other kinds of healthcare workers have demonstrated the power of healthcare worker unions. After publishing a report in 2019 that found that Johns Hopkins Hospital in Baltimore sued hundreds of patients, including low-wage employees, each year over unpaid debts, National Nurses United helped lead a campaign demanding a halt to the practice, a campaign that led to the passage of some of the strongest protections for patients in medical debt ever to be enshrined in state law. And while healthcare executives denounce unions as inappropriate for medicine, a recent econometric analysis demonstrated a causal link between unionization of nurses in nursing homes and decreased mortality rates among residents. Organizing doesn’t just benefit our own working conditions. It can improve the lives of patients, too.
Doctors in specialty training have already heeded these lessons. This year alone, votes to unionize resident physicians have been passed in landslide elections at some of the largest academic hospitals in the country, including Mass General Brigham in Boston, Montefiore Medical Center in New York, George Washington University Hospital in Washington, D.C., and Penn Medicine in Philadelphia. While self-employed physicians are barred by federal antitrust laws from bargaining collectively about reimbursement (though one of the few remaining powers of organized medicine is determining the distribution of Medicare reimbursement among specialties) these restrictions do not apply to physicians who are employees. Physicians can also join existing organizations devoted to building a more just healthcare system, organizations like Physicians for a National Health Program or the Debt Collective.
Such collective power of physicians can advance safer conditions for patients and workers, but only if it remains devoted to the principles of democratic organization and collaboration with other labor unions and patient advocates. Hospitals have, in recent years, too often marshaled their lobbying power to fight alongside the extractive middlemen of medicine against overdue reforms like single-payer health care or even requirements for charitable care in return for tax exemptions. If, in contrast, physicians maintain our alliance with patients and other healthcare workers—an alliance strengthened by the jarring and painful experiences of the Covid pandemic—physician organizations can be a powerful force for justice in healthcare. Medicine can remain a vocation—labor that is infused with purpose and dedication—but it cannot be what it was. Let’s turn the death of a profession into the birth of something new and better.