The Covid-19 pandemic continues, but funding for vaccines, tests, ventilation, and treatment does not. The United States has suffered a higher death rate than other high-income countries throughout the pandemic. The toll has also been profoundly unequal—borne disproportionately by people who are low-income, Black, Latinx, or Indigenous. And the current lack of funding from Congress is worsening access to vaccines, tests, and treatments for those who need them most. Congress must step up to ensure that all Americans have the means to protect their own and their families’ health during the pandemic—and to reduce the burden on the hospitals and health care workers we all may need in future surges.
People with low incomes have been disproportionately exposed to Covid-19 and at higher risk of severe Covid illness since the start of the pandemic. They are also more likely to be uninsured compared with their higher-income counterparts because of limited affordable health insurance coverage, frequent lack of health insurance benefits associated with low-wage jobs, and stringent Medicaid eligibility criteria in certain states.
With the end of the federal Covid reimbursement program for the uninsured on March 22, people who are uninsured have not had access to free vaccines, testing, and treatment. The latest funding deal includes funds for purchasing Covid-19 therapeutics, tests, and vaccines—tools essential tools for protecting all Americans; however, it leaves out a sizable segment of the population—those who are uninsured. Twenty-eight million uninsured Americans now have fewer options for vaccination.
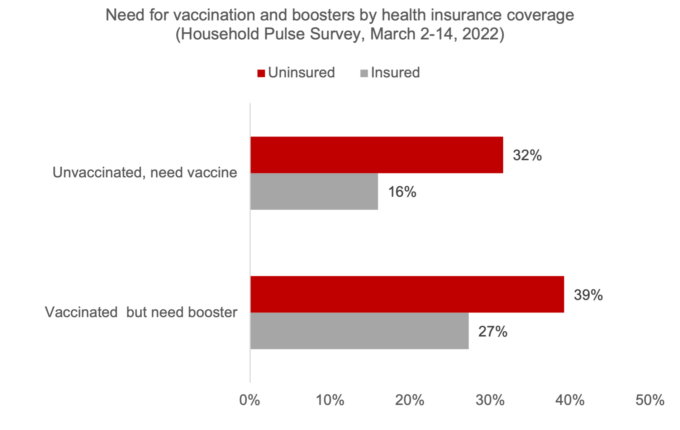
Based on analyses of a nationally representative Household Pulse Survey collected by the US Census Bureau, more than 70 percent of people who do not have health insurance needed a vaccine or booster in March 2021, and only 43 percent of people with health insurance.
Popular
"swipe left below to view more authors"Swipe →
With additional funding, Congress has the power to preserve access to vaccination for all and to counter vaccine inequities that have persisted throughout the pandemic. Recent data from Massachusetts found a strong association between median household income and booster coverage throughout the state. A lack of continued funding will likely worsen these differences as well as those related to severe Covid outcomes by income and race. Continued outreach in low-income communities, including multilingual efforts through trusted messengers, must continue to help vaccinate and boost people where they are. Distributing tests, masks, and vaccines in one place can help increase access.
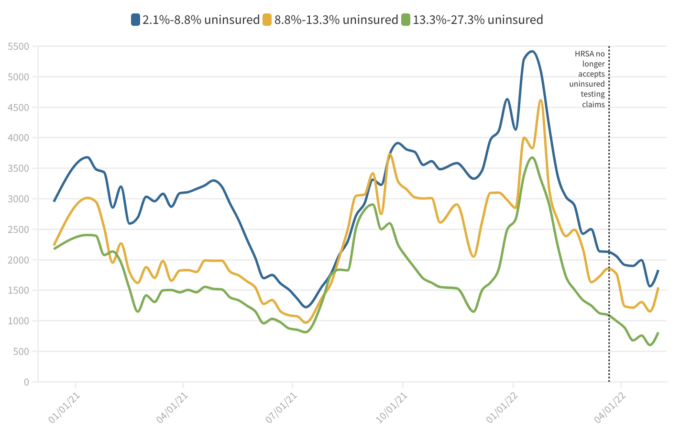
Testing remains a critical component of the US pandemic response, and Congress must continue to invest in testing. There is already lower access for people who are uninsured in many areas. For example, Embry Health, a major provider of Covid-19 testing in Arizona and neighboring states, started charging uninsured residents $100 per PCR test (at this moment, CVS and Walgreens still offer testing at no cost). With fear of hidden costs, many in low-income communities will likely be less willing to get tested, worsening our ability to reduce and to track the spread of this virus and its effects on Americans. In addition to helping slow the spread of SARS-CoV-2 within households and workplaces, testing helps minimize the chance of serious outcomes by ensuring that people who test positive can seek care if they show worsening symptoms. Testing is an important part of the test-to-treat initiative, as many providers will prescribe antivirals such as Paxlovid only with documentation of a positive test. When comparing weekly testing rates by insurance coverage status, based on the Department of Health and Human Services’s county-level Community Profile Reports, individuals living in counties with high proportions of uninsured people have testing rates of around half of those in areas with higher insurance coverage.
The lack of funding also puts an additional burden on safety net institutions such as federally qualified health centers, community clinics, and other organizations who rely on federal, state, or local government funding to continue their services and provide for the communities they serve. In the absence of reimbursement for these providers, many have been forced to lay off workers or terminate programs, further exacerbating access issues.
Making investments to expand the supply of treatments is also essential to ensuring that the chance of severe outcomes is lessened among those most at risk. Congress must maximize the reach of the test-to-treat program through funding the purchase of treatment courses and public education campaigns to encourage their use by all of those who would benefit from them. Multiple surveys show that low-income Americans, as well as those who are uninsured, have been more likely to report caring for a sick family member or missing work because of illness. Enhancing the options for early treatment, including increasing online accessibility to appointments and awareness of therapeutics, can help minimize missed work days and protect people from severe disease.
Equity must be at the forefront of the continued pandemic response. States, counties, cities, and localities need the funding to provide for the most vulnerable. Previous waves have continuously had a disproportionate effect on low-income and uninsured Americans, and more funding from Congress is imperative to closing the accessibility and affordability gap.